Changelog
RSS Feed
Subscribe to email updates:
Trusted by the fastest-growing healthtech companies
Feb 5, 2026
Claims
Electronic Remittance Advice (ERA) enrollments for the Stedi Test Payer (Payer ID: STEDITEST) now go live automatically.
You can submit claims to the Stedi Test Payer to generate realistic ERAs as part of a test workflow. To receive these test ERAs, you must first submit an ERA enrollment request for the Stedi Test Payer.
Previously, these enrollments only went live after an ERA was generated, which required submitting a claim before enrollment was active.
Now, ERA enrollments for the test payer move to the LIVE enrollment status about a minute after you submit the enrollment request.
Feb 5, 2026
Claims
Stedi now rejects 837P professional and 837D dental claims that contain invalid place of service codes.
How the edit works
Place of service codes are two-digit codes that indicate where a service was delivered. The Centers for Medicare and Medicaid Services (CMS) maintains a list of valid place of service codes. For example: 11 (Office) or 23 (Emergency Room – Hospital).
If a professional or dental claim includes an invalid place of service code, the payer may reject the claim. This can delay payment for the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s Claim Submission API endpoints, you’ll get back an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Feb 5, 2026
ERAs & transaction enrollment
You can now see how long transaction enrollment takes – minutes, hours, days, or weeks – for all Stedi payers and transaction types that require enrollment.
For payers and transaction types that don’t require enrollment, no timeframe is shown.
You can view enrollment timeframes using the Payers API or the Stedi Payer Network. For example, in the Stedi Payer Network:
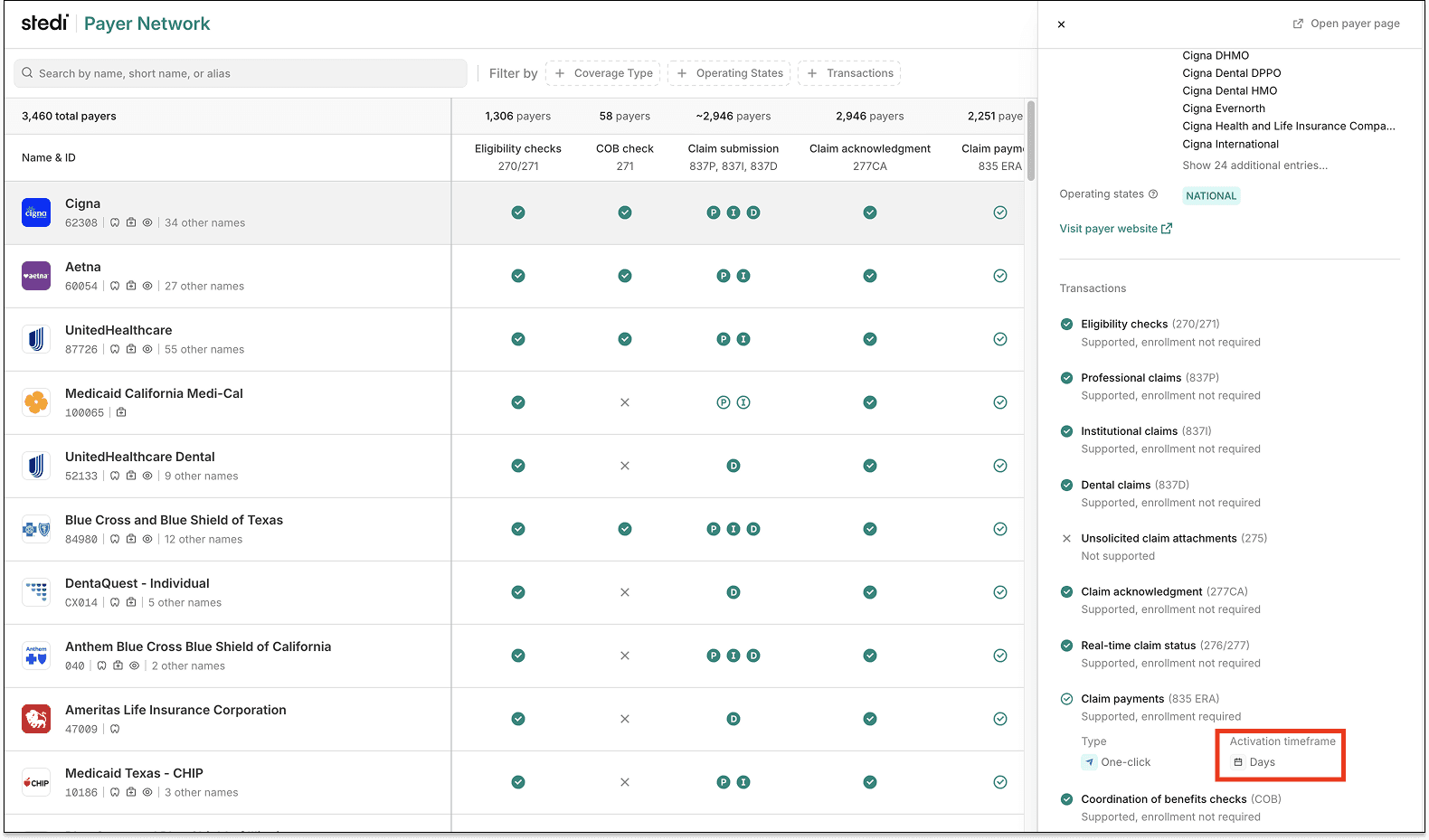
Enrollment timeframes are based on Stedi's operational data – using real enrollments completed through our platform – and payer-specific rules.
Previously, enrollment timeframes were available but not populated for every payer.
You can use enrollment timeframes to plan go-live dates and set realistic expectations with providers.
To learn more, see our Introducing timeframes for transaction enrollments blog post.
Feb 4, 2026
Eligibility checks
You can now run Medicare Beneficiary Identifier (MBI) lookups – with or without a Social Security Number (SSN) – using a CSV batch eligibility check.
Previously, batch eligibility CSVs didn't support some address or SSN fields required for MBI lookups. We've now added several new supported fields to batch eligibility CSVs.
New fields for batch eligibility CSVs
With this update, batch CSVs now support the following fields.
Provider:
providerReferenceIdentification
Subscriber:
subscriberSsnsubscriberGendersubscriberSuffixsubscriberAddress1subscriberAddress2subscriberCitysubscriberAddressStatesubscriberPostalCode
Dependent:
dependentMiddleNamedependentSsndependentGenderdependentSuffixdependentAddress1dependentAddress2dependentCitydependentAddressStatedependentPostalCode
For more information, see our batch eligibility docs.
Required fields for MBI lookups
With Stedi, you run MBI lookups as eligibility checks with the respective MBILU (MBI Lookup with SSN) or MBILUNOSSN (MBI Lookup without SSN) payer IDs. You can now run these checks using batch eligibility CSVs.
Note: MBI lookups require setup through transaction enrollment. See our related documentation.
MBI lookup with an SSN
To run an MBI lookup with an SSN, you must provide:
The patient’s first name –
subscriberFirstNameordependentFirstNameThe patient’s last name –
subscriberLastNameordependentLastNameThe patient’s date of birth –
subscriberDateOfBirthordependentDateOfBirthThe patient’s Social Security Number (SSN) –
subscriberSsnordependentSsn
MBI lookup without an SSN
To run an MBI lookup without an SSN, you must provide:
The patient’s first name –
subscriberFirstNameordependentFirstNameThe patient’s last name –
subscriberLastNameordependentLastNameThe patient’s date of birth –
subscriberDateOfBirthordependentDateOfBirthThe patient’s U.S. state –
subscriberAddressStateordependentAddressState
What to include in MBI lookups
In an eligibility check, the patient may be the subscriber or a dependent. Generally, if the dependent has their own member ID, we recommend providing their information as a subscriber.
We don't recommend including more patient demographic information, such as additional address data, than what's required. Doing so can lower MBI lookup success rates.
For more information, see our MBI lookup docs.
Jan 28, 2026
ERAs & transaction enrollment
You can now control how enrollment records are ordered in List Enrollments API responses using the sortBy query parameter.
Previously, List Enrollments API results were always ordered by createdAt in descending order. That remains the default.
With the new sortBy query parameter, you can now also sort by other fields and set a stable fallback when values are the same. For example, you can sort by statusLastUpdatedAt and fall back to id to ensure consistent, deterministic ordering:
How the sorting works
Each sortBy value uses the property:direction format. If you provide multiple sortBy values, results are sorted in the order they appear.
When you provide a single sortBy value, Stedi automatically adds id as a secondary sort in the same direction. For example, if you provide ?sortBy=updatedAt:desc, Stedi automatically adds id:desc to the query to ensure deterministic results.
To see available sortBy properties, check out our API reference documentation.
Jan 28, 2026
Eligibility checks
You’ll now get a clear warning in eligibility responses when a required member ID is missing.
Why some payers require member IDs
For eligibility checks, payers can only return coverage when the patient information in the check matches exactly one member in the payer system. To enforce this, many payers require that checks include the patient’s member ID.
When the member ID is required but missing, the payer returns a AAA error, such as 72 (Invalid/Missing Subscriber/Insured ID). These errors are generic and don’t specifically indicate the payer requires a member ID.
Stedi’s new missing member ID warning
Stedi’s new warning indicates the payer requires a member ID for patients in eligibility checks, based on Stedi’s curated sources.
The warning is returned in the warnings array, alongside the AAA error, for eligibility responses from the following endpoints:
For example, the following warning indicates the payer requires the patient’s member ID:
The warning is also shown for eligibility responses in the Stedi portal.
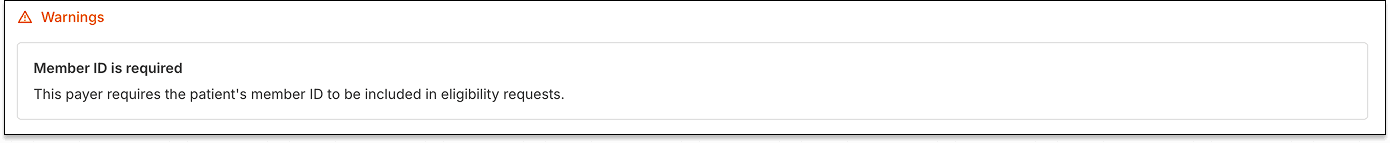
Eligibility check requirements vary by payer. If Stedi doesn't know if a payer requires a member ID for eligibility checks, no warning is returned.
For more tips and details, check out Stedi’s Eligibility troubleshooting docs.
Jan 28, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when the subscriber address or demographics are missing and the subscriber is the patient.
Subscribers and patients
In healthcare claims, the subscriber is the person who carries the insurance policy. They’re also called the insured or the primary policyholder.
The subscriber may be different from the patient – the person who receives care – or they may be the same person.
In healthcare claims, a person’s demographics are their date of birth and gender.
When the subscriber address and demographics are required
HIPAA-mandated X12 states that the subscriber’s address and demographics are required when the subscriber is the patient. Payers will use this information to verify the patient’s eligibility. If you submit a claim without this information, the payer may reject the claim, which can delay payment to the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Note: If the subscriber is not the patient, the subscriber’s address and demographics are optional.
Rejection errors
If you submit a claim that fails the edit using Stedi’s Claim Submission API, you’ll get back an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Jan 27, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that include a U.S. or Canadian address without a ZIP or postal code.
X12 states that when an address is in the United States or Canada, a ZIP or postal code is required. If it isn’t, the payer may reject the claim, which can delay payment to the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s JSON or X12 Claim Submission API endpoints, you’ll get back an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Addresses outside the U.S. and Canada
If an address is not in the U.S. or Canada, ensure the claim includes the correct country code for the address.
For example, for an 837P professional claim’s billing provider’s address, you can use the billing.address.countryCode field in JSON 837P Professional Claims API endpoint.
Jan 23, 2026
Eligibility checks
You can now control how long Stedi retries checks that failed due to payer connectivity issues when submitting batch checks using a CSV upload in the Stedi portal.
When creating a new CSV batch from the portal’s Batch eligibility checks page, click Advance options to set the Retry duration.

Retry windows can be set from 8 to 24 hours. The default is 8 hours.
For details on how retries for batch eligibility checks work, see our Batch eligibility check docs.
Jan 22, 2026
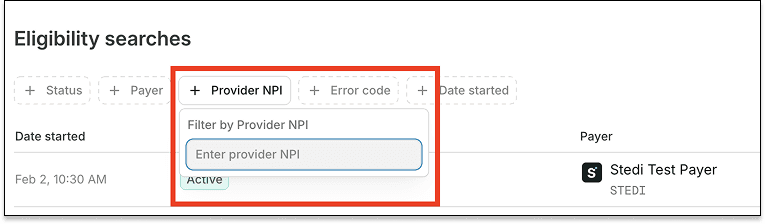
Eligibility checks
You can now filter eligibility checks – grouped as eligibility searches – by NPI on the Eligibility searches page in the Stedi portal.
A National Provider Identifier (NPI) is a unique 10-digit ID assigned to every U.S. healthcare provider by the Centers for Medicare & Medicaid Services (CMS). This filter lets you view eligibility checks associated with a specific provider.
Jan 22, 2026
Claims
If you try to submit a claim with electronic attachments to a payer who doesn't support them, Stedi now blocks the request before it reaches the payer. This affects 837P professional, 837D dental, and 837I institutional claims.
Electronic claim attachments let you send supporting documents – like X-rays and medical records – alongside claims in Stedi. Stedi lets you submit claims and claim attachments electronically using JSON API, X12 API, or SFTP.
However, not every payer supports electronic claim attachments. Previously, if you submitted an attachment to a payer who didn’t support them, the payer would reject the attachment as an error downstream. This could delay payment for the provider.
Now, Stedi checks payer support upfront and catches the issue before the claim reaches the payer. That means faster turnaround times for errors – and faster payments for providers.
Errors
If you submit a claim with attachments to an unsupported payer using Stedi's JSON or X12 Claim Submission APIs, you'll receive an error response with a 400 Bad Request HTTP status code and an error message:
If you submit a claim with attachments to an unsupported payer using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment:
Check payer support
To avoid errors, check whether a payer supports electronic claim attachments using the Stedi Payer Network site or Stedi’s Payers API.
For example, in a Search Payers API response:
Jan 22, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain a patient control number (PCN) longer than 20 characters.
What is a patient control number?
A patient control number (PCN) is a tracking ID for a claim.
You create a PCN when you submit a claim. The payer sends the ID back in follow-up transactions: claim acknowledgments, Electronic Remittance Advice (ERAs), and claim status checks.
How the edit works
HIPAA-mandated X12 states that PCNs can be up to 20 characters. If you submit a claim with a PCN longer than 20 characters, the payer may reject the claim, which can delay payment to the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s JSON or X12 Claim Submission API endpoints, you’ll get back an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Resolution tips
Follow these best practices when creating PCNs:
Stick to 17 characters.
X12 states patient control numbers can be up to 20 characters. But some payers cut off values longer than 17 characters in ERAs and claim acknowledgments.Use a unique patient control number for each claim.
If multiple claims have the same patient control number, you may match the claim to the wrong ERA or acknowledgment.Use alphanumeric characters only.
Patient control numbers can contain both letters and numbers. Avoid special characters. Many payers don’t handle them properly.Use random strings.
Predictable formats, like {patientInitials}-{DOS}, can create duplicates.
Our recommendation: Use nanoid or a similar library to create a strong, unique 17-character patient control number for each claim.
Jan 22, 2026
Claims
When you submit an 837P professional claims using the Stedi portal’s CMS-1500 form, Stedi now autocompletes patient addresses entered in Box 5 - Patient address.
Jan 22, 2026
ERAs & transaction enrollment
You can now programmatically upload, download, and delete documents for transaction enrollment requests using Stedi’s new Transaction Enrollment API endpoints:
Only PDF documents are supported.
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange a specific type of healthcare transaction with a payer.
Transaction enrollment is always required for Electronic Remittance Advice (ERAs). For other transaction types, like eligibility checks and claim submissions, enrollment requirements vary by payer.
Stedi offers fully managed, API-based transaction enrollment. You can submit and track enrollment requests using Stedi’s Transaction Enrollment API or the Stedi portal, which also supports bulk CSV imports.
When possible, Stedi handles all enrollment paperwork for you and your provider. When we can’t, we give you updates and clear next steps for what’s needed next.
What are enrollment documents?
Enrollment requirements vary by payer. Some payers require additional documents, such as:
A form with a wet signature
A practice W-9
A voided check
In these cases, Stedi updates the enrollment status to PROVIDER_ACTION_REQUIRED and notifies the submitter by email. You can then view next steps and upload the required documents through the Stedi portal or API.
Upload an enrollment document
Previously, you could only upload enrollment documents using the Stedi portal. Now, you can also upload them programmatically using the Upload Enrollment Document endpoint:
Call the Upload Enrollment Document endpoint with the enrollment ID for the enrollment request.
The enrollment ID is returned in the responses for the Create Enrollment and List Enrollments endpoints. It's also listed at the top of the enrollment's details page in the Stedi portal.
Include the PDF’s file name, including the.pdffile extension, in the request body’snamefield:The endpoint returns a pre-signed URL for uploading the PDF. The URL expires in 24 hours.
Make a
PUTrequest to the pre-signed URL to upload the PDF. Set theContent-TypeHTTP request header toapplication/pdf.Uploaded documents are listed on the enrollment's details page in the Stedi portal.
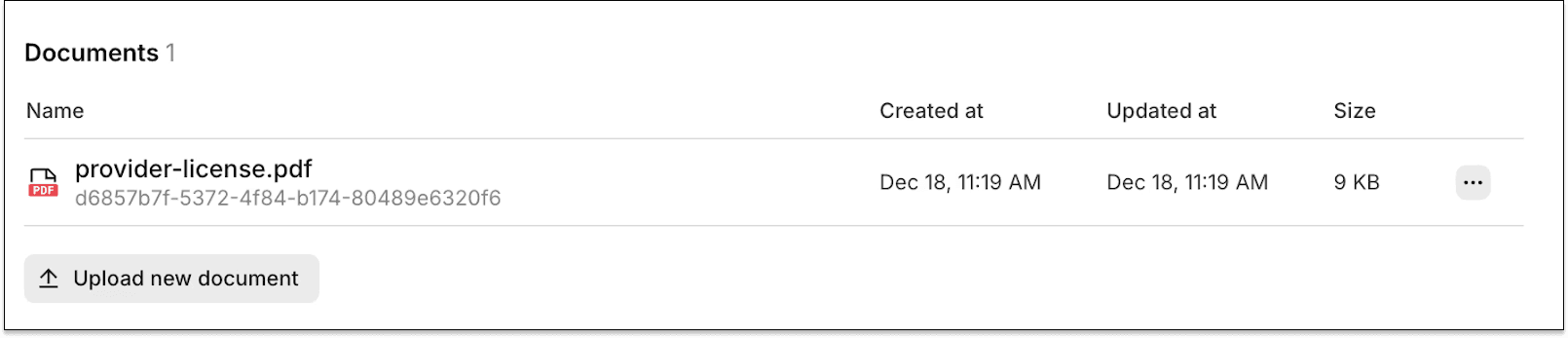
Download and delete enrollment documents
In addition to uploading, you can also download and delete previously uploaded documents using the respective Download Enrollment Document and Delete Enrollment Document endpoints.
Get started
Stedi’s Transaction Enrollment API, including the new enrollment document endpoints, is available on the Developer plan and above.
For complete details, check out our API reference documentation.
Jan 21, 2026
Claims
Stedi now rejects 837P professional and 837I institutional claims that list a sequela code as the only or primary ICD-10-CM diagnosis code.
ICD-10-CM diagnosis codes
In healthcare claims, diagnosis codes describe what’s wrong with the patient. HIPAA requires that professional and institutional claims only use valid, billable ICD-10-CM codes as diagnosis codes. For example, M54.5 is the ICD-10-CM code for “Chronic low back pain.”
A claim can include multiple diagnosis codes, listed in order of importance. The primary diagnosis code is in position 1, the next is in position 2, and so on.
Sequela codes
A sequela code is an ICD-10-CM diagnosis code used to describe a condition that remains after an earlier injury or illness has healed.
For example, M48.40XS (Fatigue fracture of vertebra, site unspecified, sequela of fracture) is a sequela code. Sequela codes always have S as the seventh character.
How the edit works
ICD-10-CM guidelines disallow a sequela code from being used as the primary or only diagnosis on professional or institutional claims. If it is, the payer may reject the claim, which can delay payment for the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
A sequela code can still be billed, as it provides additional context for the payer on why the patient has the current conditions. But those current conditions must be billed as the primary diagnosis, which describes the primary reason for service.
Rejection errors
If you submit a claim that fails the edit using Stedi’s JSON or X12 Claim Submission API endpoints, you’ll get back an error response in real time. The response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Resolution tip
In most cases, you can pass this edit by reordering the diagnosis codes so the current condition comes first and the sequela code(s) are listed afterward.
For example, M54.5 (Chronic low back pain) should be listed before the sequela, M48.40XS (Fatigue fracture of vertebra, site unspecified, sequela of fracture). Sequela codes should always accompany a preceding diagnosis code.
Jan 21, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that don’t contain one of the following IDs for the billing provider:
National Provider Identifier (NPI), a unique 10-digit identifier for the provider assigned by the Centers for Medicare & Medicaid Services (CMS)
Tax identification number (TIN), such as an Employer Identification Number (EIN) or Social Security Number (SSN)
A secondary identification number, such as a:
Payer Identification Number
Employer's Identification Number
Claim Office Number
National Association of Insurance Commissioners (NAIC) Code
The billing provider is the person or organization, such as a clinic or group practice, that will receive payment from the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s JSON or X12 Claim Submission API endpoints, you’ll get back an error response in real time. The response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Jan 19, 2026
Accounts
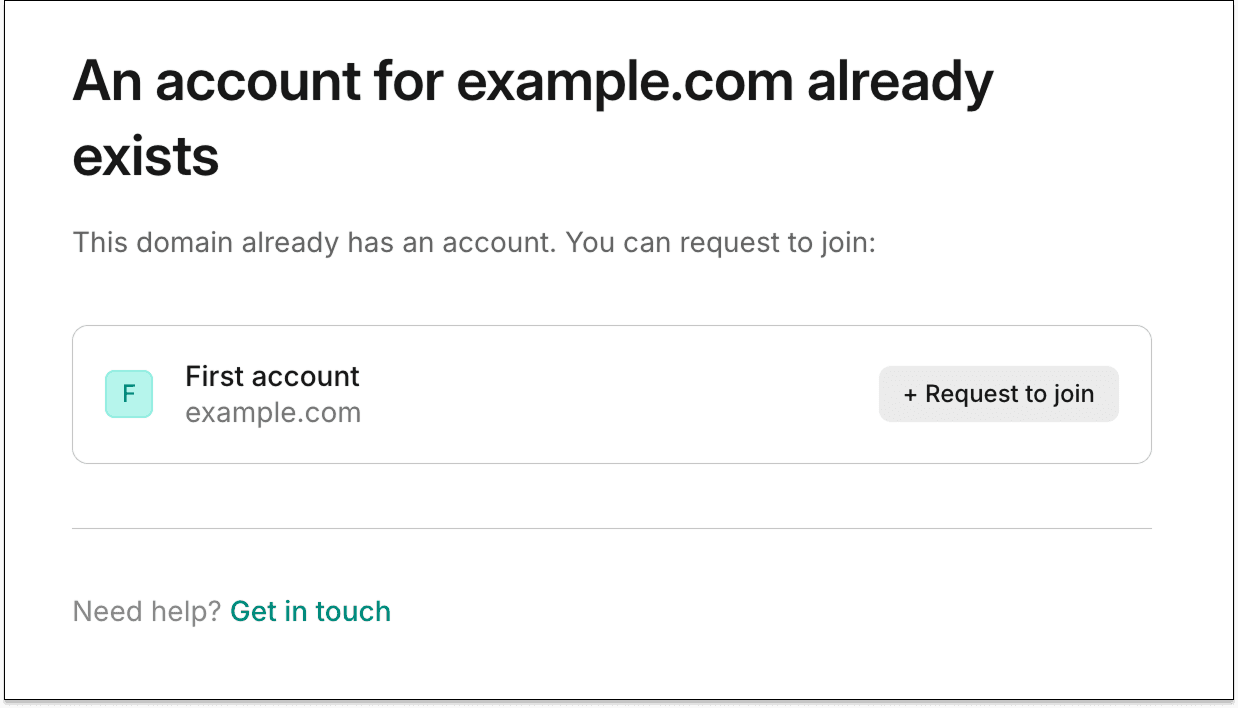
Now, when you sign up for Stedi, we check if your email domain is already tied to an existing account. If it is, you can request to join that account instead of creating a new one.
For example, if you sign up with john.doe@example.com and your company already has a Stedi account for example.com, you’ll see the option to request to join it. This helps avoid duplicate Stedi accounts for the same organization.
Jan 19, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain an invalid individual relationship code for the subscriber.
Individual relationship codes
In a healthcare claim, the subscriber is the person who holds the insurance policy. The subscriber is also called the policyholder or primary cardholder.
The subscriber is not always the patient. For example, a dependent, such as a spouse or child, may receive care through an employee’s insurance. In that case, the employee is the subscriber, even though they’re not receiving care.
Claims indicate the relationship between the subscriber and the patient using an individual relationship code in the subscriber’s section. This code tells the payer whether the patient is the subscriber themselves or a dependent covered under the same plan.
How the edits work
In a claim, if the subscriber’s individual relationship code is 18 (Self), it means the subscriber is the patient. In these cases, the claim must not include information for a dependent. Similarly, if a claim does not include a dependent’s information, the subscriber’s individual relationship code must be 18.
If a claim mixes the subscriber’s individual relationship code and dependent information incorrectly, payers may reject the claim. This can delay payment for the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Where to find the subscriber’s individual relationship code
JSON API
Professional claims JSON endpoint: claimInformation.otherSubscriberInformation[].individualRelationshipCode
Dental claims JSON endpoint: claimInformation.otherSubscriberInformation[].individualRelationshipCode
Institutional Claims JSON endpoint: claimInformation.otherSubscriberInformation.individualRelationshipCode
Raw X12
Professional claims:
SBR02(Individual Relationship Code) ofLoop 2000B(Subscriber Hierarchical Level)Dental claims:
SBR02(Individual Relationship Code) ofLoop 2000B(Subscriber Hierarchical Level)Institutional claims:
SBR02(Individual Relationship Code) ofLoop 2000B(Subscriber Hierarchical Level)
Stedi portal
Professional claims using the CMS-1500 form: Box 6 – Patient Relationship to Insured
The subscriber’s individual relationship code must not be 18
If you submit a claim with a dependent’s information and the subscriber’s individual relationship code is set to 18, Stedi’s JSON or X12 Claim Submission API endpoints return an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
The subscriber’s individual relationship code must be 18
If you submit a claim without a dependent’s information and the subscriber’s individual relationship code is missing or not set to 18, Stedi’s JSON or X12 Claim Submission API endpoints return an error response in real time. The response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Jan 16, 2026
ERAs & transaction enrollment
We now return payer.submittedPayerIdOrAlias as an optional field in responses for the following Transaction Enrollment API endpoints:
For example, in a Retrieve Enrollment response:
You must pass a payer idOrAlias when creating an enrollment using the Create Enrollment endpoint. Previously, responses only returned the stediPayerId, the Stedi payer ID that the submitted payer ID or payer ID alias resolved to.
If you submitted a primary payer ID or another payer ID alias, this made it difficult to reconcile the response with the payer ID you originally provided.
Now, submittedPayerIdOrAlias returns the payer ID or payer ID alias you submitted in the original Create Enrollment request.
Jan 15, 2026
Eligibility checks
Stedi now generates and returns a universally unique ID (UUID) for every eligibility check.
The check ID is returned in the id field of the following API responses:
The check ID is a string that always starts with ec_. For example:
For SOAP Real-Time Eligibility Check API responses, the check ID is returned in the stedi-id HTTP response header:
The check ID gives you a stable handle for a single eligibility check. You can use it to:
Track eligibility checks for debugging and troubleshooting in your application
Construct deep links to eligibility checks in the Stedi portal
Share a reference to a specific eligibility check with Stedi support
For more information, check out our announcement blog.
Jan 14, 2026
Claims
You can now include unsolicited claim attachments when submitting 837I institutional claims through Stedi’s Institutional Claims JSON API endpoint.
Previously, you could only submit attachments for institutional claims using our X12 API endpoint or SFTP.
For instructions and more information, see our Claim Attachment docs.
Jan 8, 2026
Claims
Stedi now rejects 837P professional and 837D dental claims with invalid diagnosis pointers.
How the edit works
In a claim, a diagnosis code describes what’s wrong with the patient, such as tooth decay or lower back pain. A claim can include multiple diagnosis codes, listed and indexed in order of importance. The primary diagnosis code is in position 1, the next is in position 2, and so on.
A service line is a single row on a claim that bills for one specific service, procedure, or supply – such as an office visit or a dental filling.
Each service line can include a diagnosis code pointer. This pointer tells the payer why the service was provided by linking it to a specific diagnosis code. For example, this office visit (service) was provided because of lower back pain (diagnosis). Payers use this information to determine the medical necessity or clinical rationale for the service.
The diagnosis code pointer refers to the index position of a diagnosis code on the claim. For example:
If a service line uses diagnosis pointer 2, the claim must include a diagnosis code in position 2.
If a service line uses diagnosis pointer 3, the claim must include a diagnosis code in position 3.
Payers may reject claims that include a diagnosis pointer that refers to a diagnosis code position that isn’t present on the claim. These rejections can delay payment for the provider.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Where to find diagnosis codes and pointers
JSON API
Professional claims JSON endpoint:
Diagnosis codes:
healthCareCodeInformationDiagnosis pointers:
serviceLines[].professionalService.compositeDiagnosisCodePointers
Diagnosis codes:
healthCareCodeInformationDiagnosis pointers:
serviceLines[].dentalService.compositeDiagnosisCodePointers
Raw X12
Diagnosis codes:
HI(Health Care Diagnosis Code) in Loop2300(Claim Information)Diagnosis pointers:
SV1-07(Composite Diagnosis Code Pointer) in Loop2400(Service Line)
Diagnosis codes:
HI(Health Care Diagnosis Code) in Loop2300(Claim Information)Diagnosis pointers:
SV3-11(Composite Diagnosis Code Pointer) inLoop 2400(Service Line)
Stedi portal
Professional claims using the CMS-1500 form:
Diagnosis codes: Box 21 – Diagnosis or nature of illness or injury
Diagnosis pointers: Box 24e – Diagnosis codes
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Jan 7, 2026
Eligibility checks
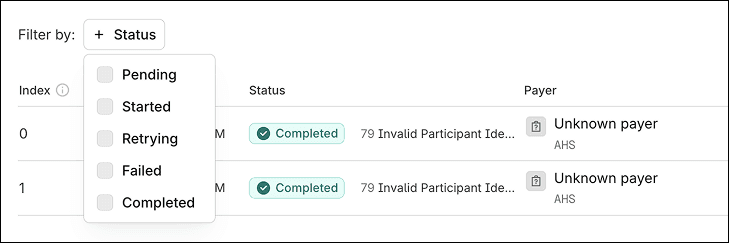
You can now filter eligibility checks within a batch by status in the Stedi portal.
Batch eligibility checks let you run multiple eligibility checks asynchronously using a single request. The checks run in a dedicated pipeline, separate from real-time checks, and Stedi handles retries for you.
You can submit batch eligibility checks through our API or by uploading a bulk CSV in the Stedi portal.
The portal’s Eligibility check batches page shows all your batch checks.
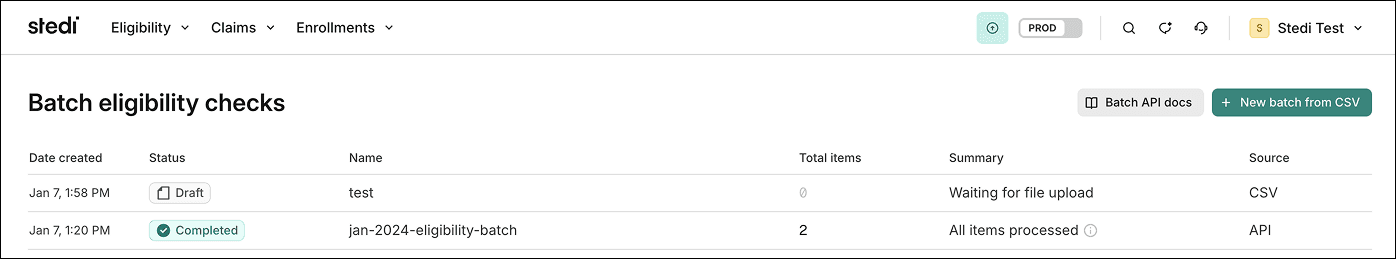
You can click a batch name to view its details, including the status – such as Started or Pending – of each check.
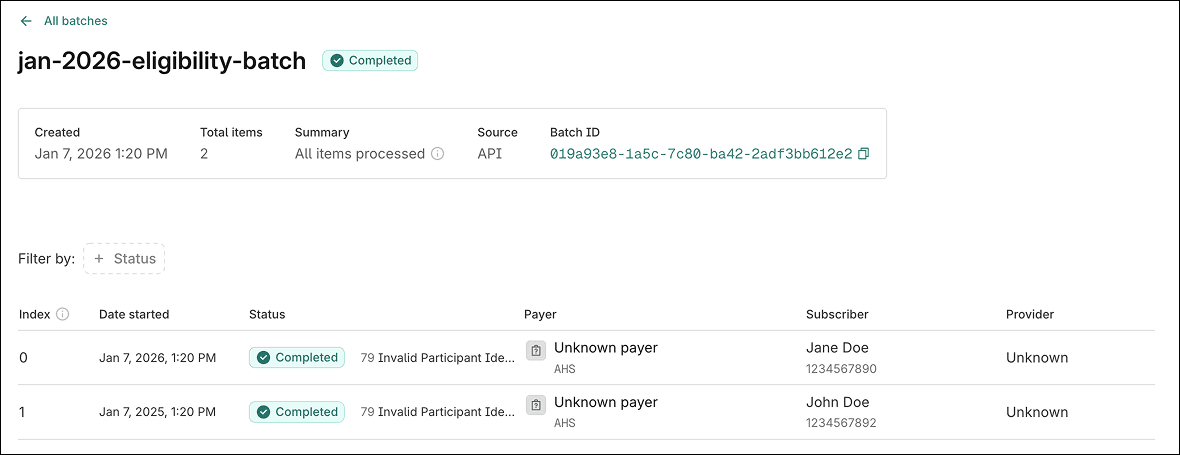
With this change, you can now filter the list based on its status.
Jan 7, 2026
Claims
You can now include the submitter’s fax number when submitting an 837P professional claim using Stedi’s CMS-1500 form.
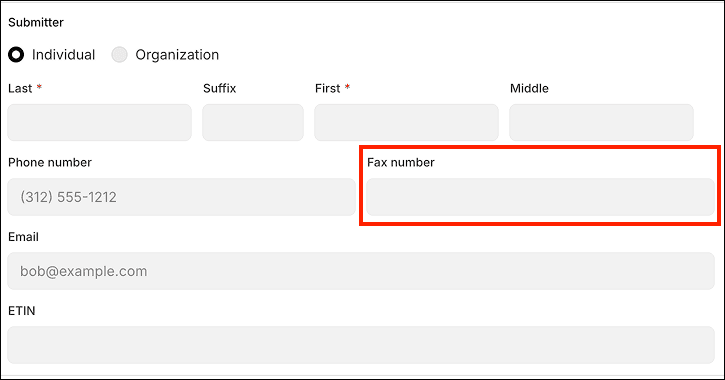
The submitter is the person or organization who creates and submits the claim. When submitting a claim, you must include at least one of the following for the submitter:
Email address
Phone number
Fax number
Payers may use this information to contact the submitter about issues with the claim. Previously, the form only accepted the submitter’s email address and/or phone number.
Jan 7, 2026
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain duplicate line item control numbers.
How the edit works
In a claim, a service line represents billing for one specific service, procedure, or supply – for example, an office visit or a dental filling. Each service line represents a separate billable event.
A line item control number is a provider-assigned identifier for a specific service line.
Within a claim, each service line must have a unique line item control number. Payers and providers use line item control numbers to track service lines across claim submissions, claim acknowledgments, and Electronic Remittance Advice (ERAs).
Payers may reject claims with duplicate line item control numbers, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
Where to find line item control numbers
JSON API
Professional claims JSON endpoint:
claimInformation.serviceLines.providerControlNumberDental claims JSON endpoint:
claimInformation.serviceLines.providerControlNumberInstitutional claims JSON endpoint:
claimInformation.serviceLines.lineItemControlNumber
Raw X12
REF-02(Line Item Control Number) of Loop2400(Service Line Number)Stedi portal
Professional claims submitted through Stedi's CMS-1500 form can’t fail this edit. You can't specify line item control numbers using the form.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will include a related claim status category code, claim status code, and error message:
Jan 6, 2026
Payers
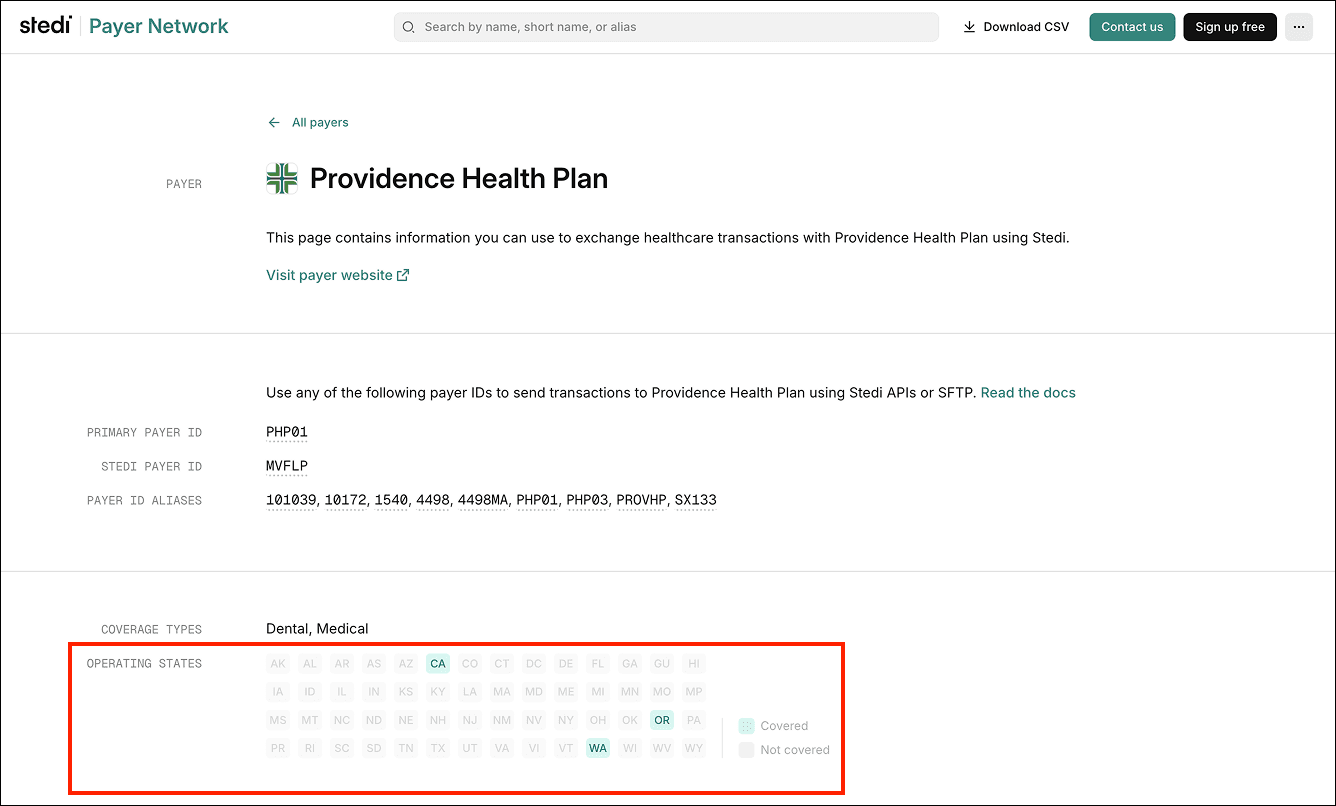
You can now see which U.S. states and territories a payer operates in using the Stedi Payer Network website and the Payers API.
Stedi payer records now list the states or territories where the payer is known or expected to offer coverage, based on Stedi’s curated sources. If Stedi doesn’t know the payer’s operating states, they aren’t included in the record.
You can also filter by operating states when searching for payers.
Filter by operating state in the Stedi Payer Network
When you browse or search payers on the Payer Network, click + Operating States beside Filter by and select one or more states. The results will use AND logic to only show payers that operate in those states.
Each payer now lists its Operating States in the Payer pane. National payers – those who cover all U.S. states display NATIONAL. Regional payers list one or more U.S. state or territory codes, such as CA (California) or WA (Washington).
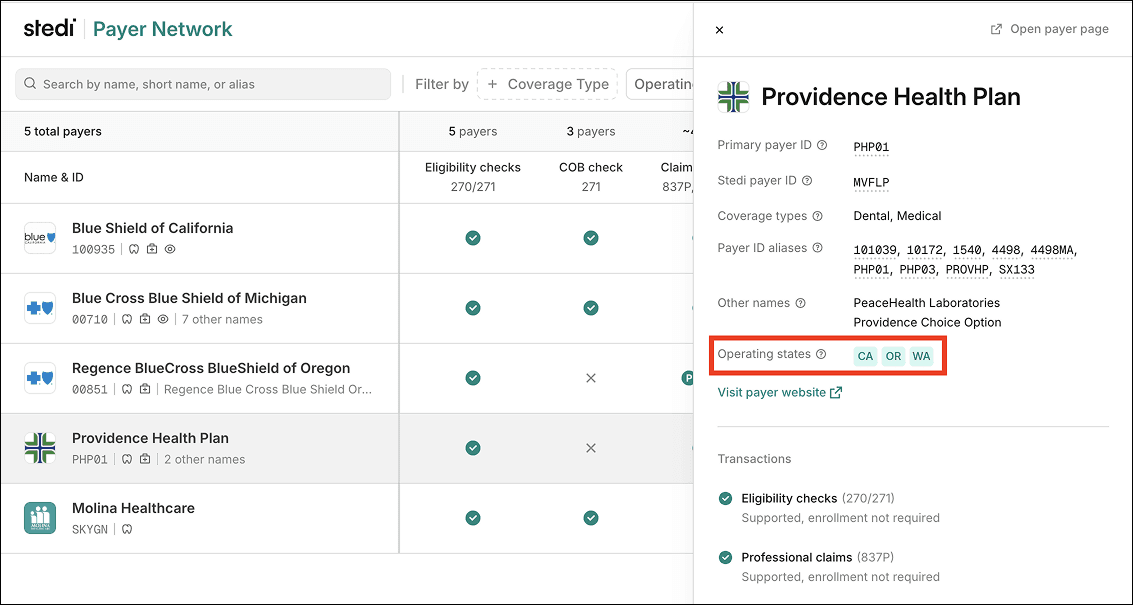
Operating states are also listed on the Payer page:
Operating states in the Payers API
All Payers API endpoints also now return an operatingStates array, if available, for payer records:
Payers that cover all U.S. states contain a single NATIONAL value in the array:
Filter by operating state using the Payers API
You can also filter payers by operating state using the Search Payers endpoint’s new operatingStates query parameter.
The parameter expects exact matches and can accept multiple values. The endpoint uses AND logic to return the intersection of all filters.
For example, the following query returns only payers that operate in both CA (California) and WA (Washington):
Jan 6, 2026
Claims
Stedi now rejects 837P professional claims when the MJ (minutes) unit of measurement code is used to incorrectly bill for anesthesia or non-anesthesia services.
In professional claims, the MJ unit of measurement code indicates a service was billed in minutes. While not a HIPAA mandate, it’s standard practice in the healthcare industry to bill for anesthesia services - but no other services – using MJ. Other services are billed using units, encounters, or time-based units – such as 15-minute increments – not raw minutes.
If MJ is used incorrectly, payers may reject the claim, which can lead to payment delays. This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When MJ must be used
If you submit a professional claim for anesthesia services that doesn't include the MJ unit of measurement code using Stedi’s 837P professional claim submission APIs or CMS-1500 professional claim form, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails this requirement using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message:
When MJ must not be used
If you submit a professional claim for non-anesthesia services that includes the MJ unit of measurement code using Stedi’s 837P professional claim submission APIs or CMS-1500 professional claim form, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails this requirement using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message:
Dec 23, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when a line item control number exceeds 30 characters.
The line item control number, also called the provider control number, is a provider-assigned identifier for each service line. Payers return this number on service lines in 277CA claim acknowledgments and 835 Electronic Remittance Advice (ERAs). Providers use it to track service lines across claim submissions, acknowledgments, and remittance files.
Line item control numbers are different from patient control numbers, which are used to track a claim as a whole.
HIPAA-adopted standards limit this line item control numbers to a maximum of 30 characters. If the value is too long, the payer may reject the claim, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A claim will fail this edit when:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, the edit fails if one of the following request field values is more than 30 characters:Professional claims JSON endpoint:
claimInformation.serviceLines.providerControlNumberDental claims JSON endpoint:
claimInformation.serviceLines.providerControlNumberInstitutional claims JSON endpoint:
claimInformation.serviceLines.lineItemControlNumber
Raw X12
If you’re using raw X12, the edit fails ifREF-02(Line Item Control Number) in any Loop2400(Service Line Number) is more than 30 characters.Stedi portal
Professional claims submitted through Stedi's CMS-1500 form can’t fail this edit. You can't specify line item control numbers using the form.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 22, 2025
Eligibility checks
You can now upload batch eligibility CSV files containing up to 10,000 checks – 10x the previous 1,000-check limit for CSV.
If you need to run more checks, you can upload and run multiple files at the same time.
For details, check out our Batch eligibility CSV upload docs.
Dec 19, 2025
ERAs & transaction enrollment
You can now programmatically retrieve PDF versions of your 835 Electronic Remittance Advice (ERAs) using Stedi’s new ERA PDF API endpoint. The {transactionId} path parameter is the ERA's transaction ID.
By default, the endpoint returns the PDF as a base64-encoded string. To get the unencoded PDF data, include the Accept: application/pdf request header. To view the PDF, save the PDF data to a file with a .pdf extension.
The PDFs are the same as the ones you can download from the Stedi portal:
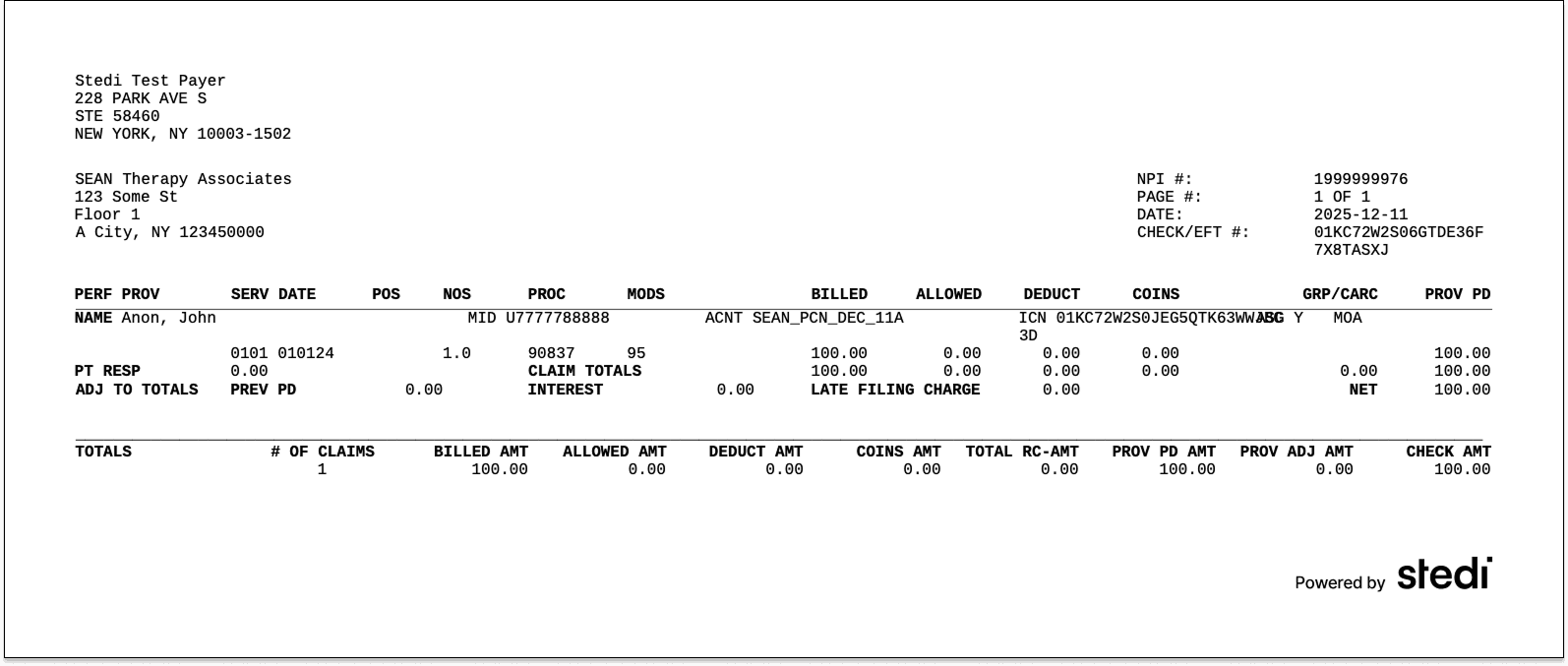
For more, check out our announcement blog or the API reference.
Dec 19, 2025
ERAs & transaction enrollment
Horizon Blue Cross Blue Shield of New Jersey (Payer ID: 22099) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 18, 2025
ERAs & transaction enrollment
You can now upload documents required for transaction enrollment requests directly in the Stedi portal. Only PDF documents are supported.
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer.
For 835 Electronic Remittance Advice (ERAs), enrollment is always required. A payer only sends ERAs to the clearinghouse the provider has enrolled with, and a provider can only enroll with the payer through one clearinghouse at a time.
Stedi offers fully-managed, API-based transaction enrollment. You can use Stedi’s enrollment API to programmatically submit and track enrollments for providers. You can also use the Stedi portal, which supports bulk CSV imports.
When possible, we handle all enrollment paperwork on your behalf. When we can’t, we let you know what’s needed next.
Upload required enrollment documents
Enrollment requirements vary by payer. Some payers require additional documents, such as:
A signed form
A practice W-9
A voided check
Previously, Stedi emailed you to request these documents and asked you to email them back to us.
With this update, we’ll still email you when an enrollment requires action. But, now, you can upload completed documents by clicking Upload new document in the Documents section of the enrollment’s details page in the Stedi portal.
The new upload functionality is available for all Stedi plans, including our free Basic plan.
For more information, see our documentation.
Dec 16, 2025
Payers
You can now get a payer’s website URL using the Stedi Payer Network and the Payers API.
Stedi payer records now list the payer’s website URL, when provided.
View payer URLs in the Stedi Payer Network
Each payer now includes a Visit payer website link, when available in the payer’s record, in the Payer pane:
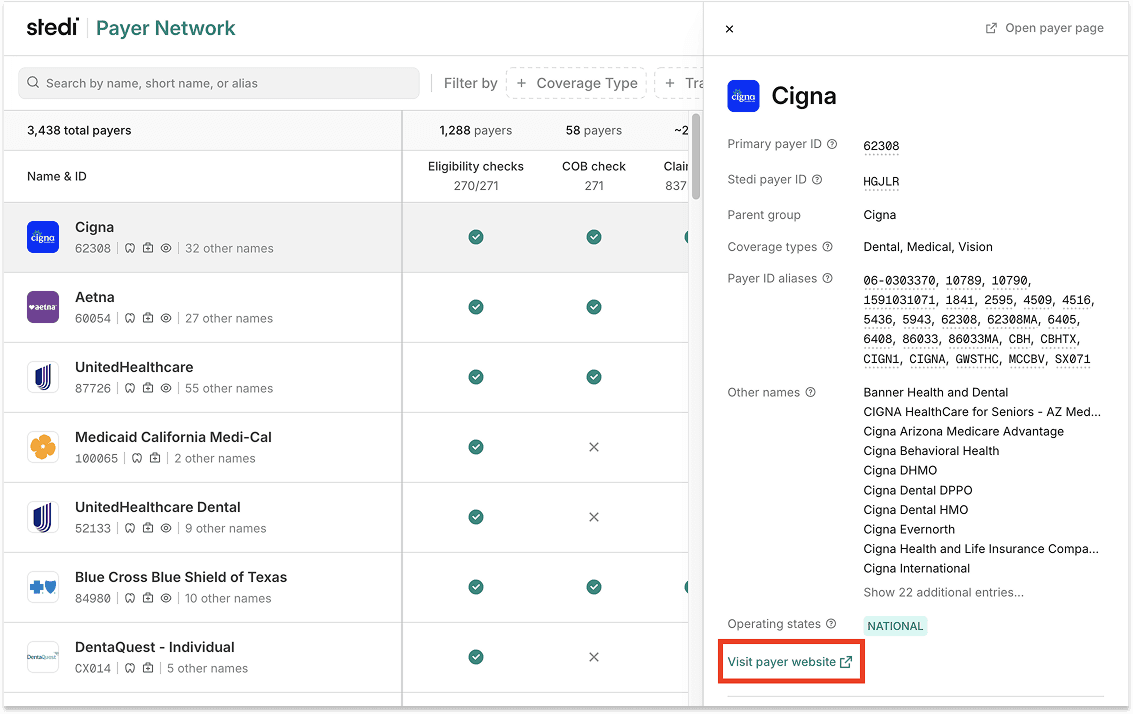
The Payer page also includes the link:
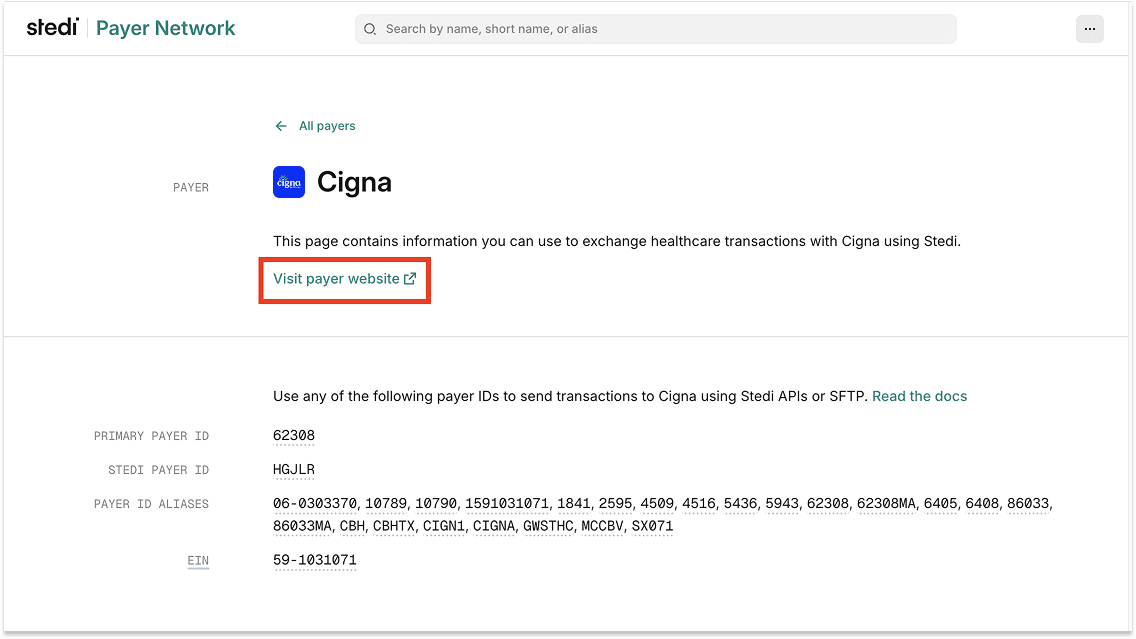
Retrieve payer URLs using the Payers API
All Payers API endpoints also now return the urls.website response property, if available, for payer records.
Dec 15, 2025
Claims
You can now correct and resubmit 837P professional claims using the Stedi portal’s CMS-1500 form.
Previously, if you submitted a claim using Stedi’s CMS-1500 form and later needed to fix it, you had two options:
Re-enter all the data into the form by hand.
Use the portal’s Edit and resubmit feature to change the raw X12.
Now, you can revise the previous claim directly in Stedi’s CMS-1500 form. Stedi loads the data from the original claim into the form for you.
For more details, see our announcement blog.
Dec 15, 2025
ERAs & transaction enrollment
You can now download unbranded ERA PDFs without a Stedi logo in the Stedi portal.
Stedi generates a PDF version of each Electronic Remittance Advice (ERA) you receive. Previously, all ERA PDFs included “Powered by Stedi” in the page footer. Now, you have the option to download ERA PDFs without this footer.
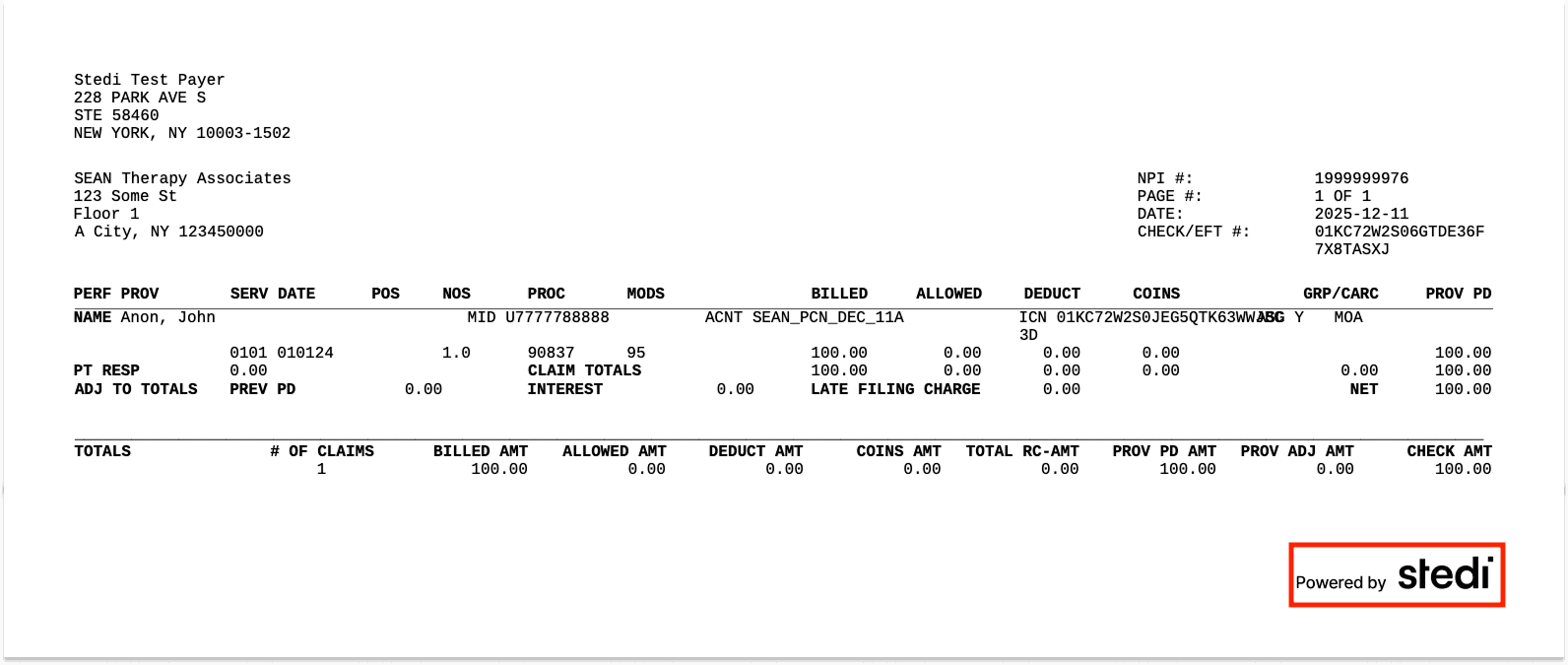
To download an unbranded ERA PDF:
Go to the Transactions page.
Click the ERA transaction you want to download.
On the Overview tab, click Fetch artifact. Then click … and select Download 835 ERA PDF without Stedi logo.
Dec 12, 2025
Claims
Stedi now rejects 837I institutional claims that are missing a required admission source code.
In an institutional claim, the admission source code tells you where the patient came from, such as the emergency room (ER), a doctor’s referral, or another facility.
Most institutional claims require this code. Without it, the payer can’t adjudicate the claim. The one exception is non-patient lab services, where no patient is present.
If the code is missing when required, the payer may reject the claim, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before the claim reaches the payer.
When this edit applies
An institutional claim will fail this edit in the following cases:
JSON API
If you’re using Stedi’s JSON institutional claim submission API endpoint, the edit fails if:The
admissionSourceCodefield is missing or empty.
ANDThe
placeOfServiceCodefield does not contain14(Non-Patient Laboratory).
Raw X12
If you’re using raw X12, the edit fails if:
Rejection errors
If you submit a claim that fails the edit using Stedi’s institutional claim submission API endpoints, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 11, 2025
Accounts
Stedi app developers can now configure their apps to automatically add one or more support users – called members – to accounts that install their app.
App developers can use the support users to provide support or help with implementation.
This new feature is optional. The support user has the Developer role.
What is a Stedi app?
A Stedi app is a prebuilt integration between Stedi and a third-party platform.
Stedi accounts on the Basic plan can install Stedi apps to quickly connect their account to a third-party Revenue Cycle Management (RCM) system, Practice Management System (PMS), Electronic Health Record (EHR) platform, or other Stedi Platform Partners.
For example, a practice or provider on Stedi’s free Basic plan can install a Stedi app to connect their Stedi account to their EHR.
As an app developer, you can choose to offer your app for free on the Basic plan or require a paid upgrade.
Get started with Stedi apps
To discuss publishing or configuring a Stedi app, contact us. You can also check out Publish your app in our developer docs.
To install a Stedi app, log in the Stedi portal and go to the Apps page. You can also check out our related docs.
Dec 11, 2025
ERAs & transaction enrollment
Priority Health (Payer ID: PRHTH) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
ERAs & transaction enrollment
Highmark Western and Northeastern New York (Payer ID: 55204) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
ERAs & transaction enrollment
Healthcare payer Quartz (Payer ID: 39180) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
ERAs & transaction enrollment
Highmark Blue Cross Blue Shield of Western New York (Payer ID: 100948) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
ERAs & transaction enrollment
Blue Cross Blue Shield of Kansas City (Payer ID: 47171) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
ERAs & transaction enrollment
Blue Cross Blue Shield of Kansas (Payer ID: 47163) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 11, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain an invalid date of birth.
In a claim, you must provide a date of birth for the patient. If the subscriber is a different person, you must also provide the date of birth for the subscriber – the person who carries the insurance policy.
Payers use dates of birth to distinguish between members with similar names. If you provide an invalid date of birth for the patient or subscriber, the payer may reject the claim, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A claim will fail this edit when the patient or subscriber’s provided date of birth:
Occurs after the claim’s transaction date. – the date the claim is submitted. Providers always submit claims after care is provided. Logically, the date of birth can’t occur after the date the claim is submitted.
If you’re using Stedi’s JSON claim submission APIs or professional claim form, this is the date you submit the claim to Stedi. In X12 claims, this date is in segmentBHT-04(Transaction Set Creation Date).
ORIndicates an age of 150 years or older
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 11, 2025
ERAs & transaction enrollment
Dentaquest - Individual (Payer ID: CX014) now supports one-click transaction enrollment for Electronic Remittance Advice (ERAs).
What is transaction enrollment?
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Payers always require transaction enrollments for ERAs.
You can submit and track enrollments using Stedi's transaction enrollment API, the Stedi portal, or a bulk CSV.
One-click enrollment
Enrollment requirements vary by payer. Some payers may require the submitter to sign PDFs or complete tasks in the payer's portal.
If a payer supports one-click enrollment, you only need to submit the enrollment request. There are no follow-up steps. Stedi handles everything else.
You can check whether a payer requires enrollment – and supports one-click enrollment – for ERAs and other transaction types using the Stedi Payer Network or the Payer APIs.
For details, see our transaction enrollment docs.
Dec 10, 2025
Claims
Stedi now rejects 837P professional and 837I institutional claims that bill for a drug or biologic without a valid unit count.
In professional and institutional claims, you bill for drugs or biologics by adding information about the drug to a service line, specifying what drug was administered and how much.
The line’s unit of measurement code – such as F2 (International Unit) or GR (Gram) – shows how the drug was measured. The line’s unit count reports the quantity administered in that measure.
Payers use the measurement code and unit count to verify dosage and pricing. Without a valid unit count, they can’t confirm the billed amount and may reject the claim, which can delay payment.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A professional or institutional claim will fail this edit in the following cases:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, the edit fails if:A service line contains a
drugIdentification.measurementUnitCodevalue.
ANDThe service line’s
drugIdentification.nationalDrugUnitCountfield is less than or equal to”0”.
Raw X12
If you’re using raw X12, the edit fails if:Loop 2410(Drug Identification) is present
ANDThe
CTP-05(Composite Unit of Measure) ofLoop 2410contains a value.
ANDThe
CTP-04(National Drug Unit Count) ofLoop 2410is less than or equal to0.
Stedi portal
If you’re using the Stedi portal’s professional claim form, the edit fails if:Box 24 – Service Lines contains a service line with a Unit/Basis of measurement value and a Quantity less than or equal to zero.
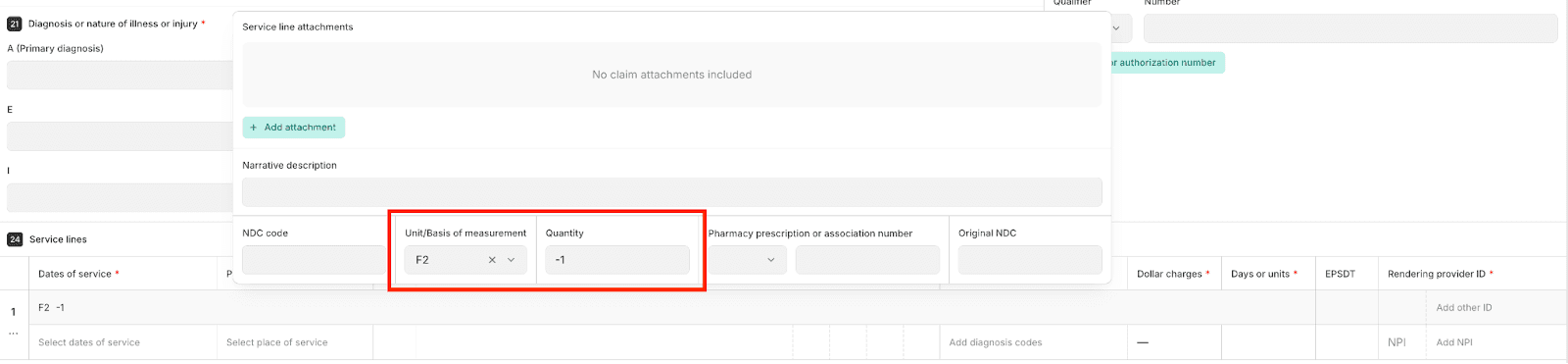
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 10, 2025
Claims
Stedi now rejects 837P professional and 837D dental claims that relate to an auto or other accident but don’t include an accident date.
When you submit a professional or dental claim, you can indicate that the patient’s condition is related to an accident using a related causes code. Valid codes are AA (Auto accident), EM (Employment), and OA (Other accident).
If you provide a related causes code of AA or OA, payers also require an accident date – the date the injury occurred. Payers use this date to determine liability, coordinate benefits with other payers, and correctly adjudicate the claim.
If you don’t include the accident date in these cases, the payer may reject the claim, which can delay payment.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A professional or dental claim will fail this edit in the following cases:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, the edit fails if:The
claimInformation.relatedCausesCodearray containsAA(Auto accident) orOA(Other accident).
ANDThe
claimInformation.claimDateInformation.accidentDatefield is empty or missing.
Raw X12
If you’re using raw X12, the edit fails if:The
CLM11-1(Related Causes Code) orCLM11-2(Related Causes Code) ofLoop 2300(Claim Information) containsAA(Auto accident) orOA(Other accident).
ANDThe
DTP-03(Accident Date) ofLoop 2300is empty or missing.
Stedi portal
If you’re using the Stedi portal’s professional claim form, the edit fails if:The Auto accident? or Other? field of Box 11 – Is patient's condition related to is Yes.
Box 15 – Other Date does not contain a Date with a Qualifier of 439 (Accident)
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 9, 2025
Claims
Stedi now rejects 837I institutional claims that contain an invalid service line revenue code.
Revenue codes are standardized, 4-digit codes that hospitals and other care facilities use to identify the type of room, service, or supply billed on a service line. Example revenue codes include:
0450– Emergency Room0360– Operating Room Services0300– Laboratory
Revenue codes are different from procedure codes, such as CPT or HCPCS codes. A procedure code describes what kind of care was delivered. A revenue code describes the type of facility associated with the charge.
Revenue codes are maintained by the National Uniform Billing Committee (NUBC). They are always 4 digits and start with a 0, 1, 2, or 3.
Revenue codes often drive how payers price and reimburse institutional claims. If a claim includes an invalid revenue code, the payers may reject the claim, which can delay payment.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
An institutional claim fails this edit if a service line revenue code:
Is not exactly 4 digits
Does not start with a
0,1,2, or3
If you're using Stedi’s JSON institutional claim submission endpoint, you provide the revenue code in the serviceLineRevenueCode field for the service line.
In raw X12, you provide the revenue code for a service line in SV2-01 (Service Line Revenue Code) of Loop 2400 (Service Line Number).
Rejection errors
If you submit an institutional claim that fails the edit using Stedi’s institutional claim submission API endpoints, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes error details in the errors array:
If you submit an institutional claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 8, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that include duplicate payer responsibility level codes.
Payer responsibility level codes, also called payment responsibility sequence number codes, indicate which payer is supposed to pay first, second, and so on. For example, a code of P indicates the primary payer. A code of S indicates the secondary payer.
The process of determining this order is known as coordination of benefits (COB). Payers use this information to process secondary and tertiary claims correctly.
If a claim lists more than one payer at the same responsibility level – for example, two primary payers – the payer may reject the claim, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A claim will fail this edit when:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, the edit fails if thesubscriber.paymentResponsibilityLevelCodefield and/or anyclaimInformation.otherSubscriberInformation.paymentResponsibilityLevelCodefields contain a duplicate value.
Raw X12
If you’re using raw X12, the edit fails ifLoop 2000B(Subscriber Hierarchical Level) and/orLoop 2320(Other Subscriber Information) contain a duplicateSBR-01(Payer Responsibility Sequence Number Code) value.
Stedi portal
You can’t fail this edit using the Stedi portal’s professional claim submission form. Currently, the form only supports claims to a single primary payer. Secondary and tertiary claims aren't supported.
This edit does not fail if a claim lists multiple payers with a responsibility level code of U (Unknown). A code of U doesn’t indicate a specific payment order, so duplicates are allowed.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 8, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that don’t include a primary payer.
Every claim must include exactly one primary payer. For primary claims, this payer determines routing. For secondary and tertiary claims, payers use this information to determine coordination of benefits (COB) and adjudicate the claim correctly. If it’s missing, the payer may reject the claim, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
When this edit applies
A claim will fail this edit when:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, the edit fails if neither thesubscriber.paymentResponsibilityLevelCodenor anyclaimInformation.otherSubscriberInformation.paymentResponsibilityLevelCodefields contains a value ofP(Primary) in the request.
Raw X12
If you’re using raw X12, the edit fails if neitherLoop 2000B(Subscriber Hierarchical Level)) norLoop 2320(Other Subscriber Information) contains anSBR-01(Payer Responsibility Sequence Number Code) value ofP(Primary).
Stedi portal
You can’t fail this edit using the Stedi portal’s professional claim submission form. Currently, the form only supports claims to a single primary payer. Secondary and tertiary claims aren't supported.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tips
For secondary and tertiary claims, include a single primary payer in other subscriber information:
JSON API
If you’re using one of Stedi’s JSON claim submission API endpoints, you can provide this information in aclaimInformation.otherSubscriberInformationobject with apaymentResponsibilityLevelCodeofP(Primary) in the request.
Raw X12
If you’re using raw X12, you can provide this information inLoop 2320(Other Subscriber Information) with anSBR-01value ofP(Primary).
Dec 8, 2025
Eligibility checks
In the coming weeks, Stedi will normalize all X12 271 eligibility responses to use a standard set of delimiters.
If you do not parse the raw X12 271 and only parse Stedi's JSON response, this change will not impact you.
What are X12 delimiters?
In X12, delimiters are characters that separate the parts of a transaction set. Each transaction set has four types of delimiters:
Element Separator – Separates fields
Repetition Separator – Separates repeat values
Component Element Separator – Separates sub-elements
Segment Terminator – Ends each segment
These delimiters are defined in the ISA segment and can vary across transaction sets.
How it works today
Stedi currently passes through whatever X12 delimiters the payer sends.
However, some payers use unsafe characters, such as carriage returns, as delimiters in their 271 eligibility responses. This can break X12 parsing for some Stedi customers.
What’s changing
Stedi will normalize all delimiters returned in X12 271 eligibility responses to the following characters:
Element Separator:
*Repetition Separator:
^Component Element Separator:
>Segment Terminator:
~
If any of the above delimiters appear in a data element value – meaning the delimiter isn’t used to delimit content but is used as content – we will replace it as follows:
Character in content | Replaced with |
|
|
|
|
|
|
|
|
For example:
What’s impacted
This change will affect all X12 271 eligibility responses returned by Stedi, including those returned by the:
x12 property of our JSON Eligibility API endpoint
x12 field of our Poll Batch Eligibility Checks endpoint
Stedi portal
Next steps
If you do not parse the raw X12 271 and only parse Stedi's JSON response, this will not impact you. Most Stedi customers won’t need to make any changes for this update.
However, if your X12 parser assumes fixed delimiters instead of reading them from the ISA segment, you should confirm that your parser will continue to work after the update.
If you need time to update your parsing logic or have questions, contact us using your dedicated support channel or our contact form by December 22, 2025.
Dec 4, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that list a non-physical address for the billing provider. Non-physical addresses include Post Office (PO) Boxes, lockboxes, private mailboxes (PMBs), and similar mailbox-only addresses.
For claims, HIPAA requires that the provider’s billing address be a physical practice location where care is delivered. If you’re using Stedi’s JSON claim submission API endpoints, this address is in the request’s billing.address field. In X12, the address is in N3 (Billing Provider Address) of Loop 2010AA (Billing Provider Name).
Payers may reject claims when the billing provider address is not a real street address, which can cause payment delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tips
If the billing provider receives mail at a PO Box, lockbox, or other non-physical address, you can provide a “pay-to” address in the claim.
If you’re using Stedi’s JSON claim submission API endpoints, you can specify the pay-to address in the request’s payToAddress field or, for institutional claims, the billingPayToAddressName field. In X12, you can specify the pay-to address in N3 (Pay-to Address) of Loop 2010AB (Pay-to Address Name).
Dec 3, 2025
Claims
Stedi now rejects 837P professional claims that are billed to Medicare Part B for chiropractic services when the primary diagnosis doesn’t indicate subluxation – a partial dislocation of a spinal joint.
Medicare requires the primary diagnosis on a chiropractic claim to indicate subluxation. In ICD-10-CM, this is represented by the M99.0x family of diagnosis codes: M99.00-M99.05.
Medicare Part B claims submitted with a non-subluxation primary diagnosis may be rejected by the Medicare Administrative Contractor (MAC) payer, which can cause delays.
This edit – the industry’s term for an automated validation rule – catches the issue before the claim reaches the MAC.
When this edit applies
A claim will fail this edit when all of the following are true:
The claim is billed to Medicare Part B.
In raw X12, this is indicated by a value of
MB(Medicare Part B) inSBR09(Claim Filing Indicator Code) ofLoop 2000B(Subscriber Information).In the JSON professional claims submission endpoint, this is indicated by a Claim Filing Indicator Code of
MB(Medicare Part B).In the professional claim form, this is indicated in Box 1 – Insurance type by a value of Medicare.
The claim includes a service line with one of the following Chiropractic Manipulative Treatment (CMT) procedure codes:
98940,98941, or98942.The claim’s primary diagnosis code is not within the M99.00-M99.05 range (inclusive).
In raw X12, the primary diagnosis is the first diagnosis code in
HI(Health Care Diagnosis Code) ofLoop 2300(Claim Information).In the JSON professional claims submission endpoint, the primary diagnosis is in the diagnosisCode field of the first object in the claimInformation.healthCareCodeInformation array.
Note: Do not include decimal points in the diagnosis code.In the professional claim form, the primary diagnosis is the first diagnosis code in Field A of Box 21 – Diagnosis or nature of illness or injury.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 3, 2025
Eligibility checks
You can now look up a patient’s Medicare Beneficiary Identifier (MBI) without a Social Security Number (SSN) using Stedi's Eligibility APIs or the Stedi portal.
Two types of MBI lookups
With this update, you can now perform an MBI lookup in two ways. Each uses a different payer ID:
Type | Payer ID | Required patient data |
MBI lookup with SSN |
| First name, last name, date of birth, SSN |
MBI lookup without SSN |
| First name, last name, date of birth, U.S. state |
Note: When running an MBI lookup without SSN using our raw X12 or SOAP eligibility endpoints, you must include a city, in addition to a U.S. state, in Loop 2100C N4. You can use a dummy city value, such as DUMMY, if needed. If you omit the city value, you'll receive an X12 validation error.
Transaction enrollment
Before running an MBI lookup without an SSN, enroll the provider for eligibility checks with the MBILUNOSSN payer ID using the Transaction Enrollment API or the Stedi portal. Enrollments for the MBILUNOSSN payer typically take 1-3 business days to complete.
You’ll get an email once the enrollment is live. You can also check enrollment status using the List Enrollments or Retrieve Enrollment API endpoints.
Run an MBI lookup without an SSN
After the enrollment is live, send an eligibility check to MBILUNOSSN. Include:
The provider’s NPI
The patient’s first name
The patient’s last name
The patient’s date of birth
The patient’s U.S. state
The patient's city (if using the raw X12 or SOAP eligibility endpoints)
For example, using Stedi’s JSON Eligibility API:
The response includes the MBI as the subscriber’s member ID. For example:
For more details, see our announcement blog.
Dec 2, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that indicate an attachment was or will be sent by mail, electronically, email, fax, or file transfer – but don’t include an attachment control number.
Some payers require supporting documents, such as X-rays or treatment plans, before approving claims for certain services. Depending on the payer, you can send attachments in several ways, including by mail or electronically using a 275 claim attachment transaction through Stedi.
When a claim indicates that an attachment was or will be sent by mail, electronically, email, fax, or file transfer, you must include an attachment control number. The payer uses this value to match the attachment to the claim.
Payers may reject claims missing this number, which can cause delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
This edit only applies when the claim indicates that an attachment was or will be sent. If the claim does not reference an attachment, this edit does not run.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 2, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain an invalid tax identification number (TIN) for the billing provider.
When you submit a claim, you must include the billing provider’s TIN – either a Social Security Number (SSN) or Employer Identification Number (EIN). The TIN must be a 9-digit number with no spaces or separators.
Payers reject claims that contain an invalid TIN for the billing provider, which can cause delays.
This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 2, 2025
Claims
You can now submit multiple claims in a single 837 transaction set using X12 over SFTP. 837P professional, 837D dental, and 837I institutional claims are supported.
Some billing platforms create a single 837 transaction set (one ST/SE segment) that includes multiple claims from different billing providers or patients. The transaction set may include claims for different payers. To deliver the claims to the correct payer, the X12 must be split into separate 837 transactions.
Stedi automatically splits 837 transaction sets containing multiple claims at the Billing Provider (2000A), Subscriber (2000B), and Claim Information (2300) loops. Behind the scenes, Stedi creates separate 837 transactions for each claim and routes them to the payer independently. Multiple claims going to the same payer will also be split to maintain the same behavior across all 837 transactions.
For example, if your 837 transaction set has two billing providers (two 2000A loops), each with three subscribers (three 2000B loops), and two claims per subscriber (two 2300 loops), Stedi submits 12 separate claim transactions.
Pricing
Stedi charges for each split claim transaction. For example, if a transaction set would result in 12 claim transactions, you're billed for 12 claim submissions. For rates, see our pricing page or contact us.
Claim acknowledgments and ERAs
The Stedi portal’s Transactions page will only display one 837 transaction, representing the original X12 file, and you’ll receive a single 999 acknowledgment. However, 277CA claim acknowledgments – from Stedi and the payer – and 835 Electronic Remittance Advices (ERAs) will reference the split 837 claims. Stedi will also run claim edits on the split 837 claims to catch rejections early.
If you submit a batch X12 claim to the Stedi Test Payer (Payer ID: STEDITEST), each transaction receives its own mock 835 Electronic Remittance Advice (ERA).
Dec 2, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that are missing the patient’s date of birth or gender.
Payers use the patient’s date of birth and gender to match the claim to the correct patient record. If either field is missing, the payer will reject the claim, which can cause delays.
This new edit – the industry's term for an automated validation rule – catches the issue before the claim ever reaches the payer.
Patient vs. subscriber vs. dependent
In a health insurance claim, there are three distinct roles:
The subscriber is the person who holds the insurance policy. They’re also called the insured, the primary policyholder, or the primary cardholder.
A dependent is someone covered under the subscriber’s plan, such as a spouse or child.
The patient can be either the subscriber or a dependent, depending on who received care.
For example, if a child receives dental care, the child is the patient even though the parent is the subscriber.
Claims must include the patient’s date of birth and gender – not just the subscriber’s – so the payer can identify the correct person.
How the edit works
A claim can include information for both the subscriber and the dependent, if applicable. You only include the dependent’s information if the dependent is the one who received care and the dependent doesn’t have their own member ID.
As part of the edit, Stedi checks the patient’s information to ensure the claim includes the patient's date of birth and gender:
If the subscriber is the patient: The edit requires the subscriber’s date of birth and gender.
If the dependent is the patient: The edit requires the dependent’s date of birth and gender and ignores the subscriber's date of birth and gender.
If the patient’s date of birth or gender is missing, Stedi rejects the claim so you can correct and resubmit it before it reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes an error in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 2, 2025
Claims
Stedi now rejects 837P professional claims that are billed to Medicare Part B for chiropractic services when the initial treatment date is missing.
Medicare requires chiropractic claims to include the initial treatment date. CMS defines this as the first date the chiropractor provided active treatment for the current episode. If that date is missing, the Medicare Administrative Contractor (MAC) payer will reject the claim, causing delays.
This edit – the industry’s term for an automated validation rule – catches the issue before the claim reaches the MAC.
When this edit applies
A claim will fail this edit when all of the following are true:
The claim is billed to Medicare Part B.
In raw X12, this is indicated by a value of
MB(Medicare Part B) inSBR09(Claim Filing Indicator Code) ofLoop 2000B(Subscriber Information).In the JSON professional claims submission endpoint, this is indicated by a Claim Filing Indicator Code of
MB(Medicare Part B).In the professional claim form, this is indicated in Box 1 – Insurance type by a value of Medicare.
The claim includes a service line with one of the following Chiropractic Manipulative Treatment (CMT) procedure codes:
98940,98941, or98942.The claim is missing the initial treatment date.
In raw X12, this is indicated by a date with qualifier
454(Initial Treatment) inDTP01(Date - Initial Treatment Date) ofLoop 2300(Claim Information).In the JSON professional claims submission endpoint, you can provide this in the
initialTreatmentDatefield.In the professional claim form, enter the date in Box 15 – Other date with a Qualifier of
454(Initial Treatment).
Rejection errors
If you submit a claim that fails the edit using Stedi’s professional claims submission API endpoints or professional claim form, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 2, 2025
Eligibility checks
The Centers for Medicare and Medicaid Services (CMS) requires that providers complete transaction enrollment to run eligibility checks through Stedi or other clearinghouses.
When an eligibility check to CMS fails with AAA error 41 – meaning the provider isn’t enrolled with CMS for eligibility transactions – Stedi now automatically submits the required transaction enrollment request. CMS usually processes these enrollments within 24-48 hours.
With this change, Stedi customers no longer need to track down and submit missing enrollments when a Medicare eligibility check fails. Stedi now handles that work for you. This reduces your operational overhead and helps ensure future Medicare checks will succeed.
For more information, see the related announcement blog.
Dec 1, 2025
Claims
Stedi now rejects 837I institutional claims that include an invalid billing provider ZIP code.
Institutional claims must include a full nine-digit ZIP code – called a ZIP+4 – with no spaces or hyphens for the billing provider. For example: 100031502. If you don’t know the full ZIP+4, you can look it up using the USPS ZIP Code Lookup tool.
If you submit institutional claims through Stedi’s institutional claim submission JSON API endpoint, this ZIP code is provided in the providers.address.postalCode field.
Payers reject claims that are missing a full ZIP+4 or that contain an invalid code, which can cause delays.
This edit – the industry’s term for an automated validation rule – prevents these claims from reaching the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s institutional claim submission API, you’ll get back an error message in real time. If you’re using the JSON API endpoint, the response includes an error in the errors array:
If you submit an institutional claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 1, 2025
Claims
Stedi now rejects 837P professional and 837D dental claims that are missing the subscriber’s member ID when the subscriber is a person.
Payers use the subscriber’s member ID to identify the patient and verify eligibility. It’s typically printed on the subscriber’s insurance card. If it’s missing, the payer will reject the claim, which delays processing.
This new edit – an industry term for an automated validation rule – catches the issue before the claim ever reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes an error in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tip
Add the subscriber’s member ID and resubmit the claim. If you’re using Stedi’s JSON API endpoints, provide this value in the subscriber.memberID field.
Dec 1, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when an adjustment amount is zero.
In healthcare claims, an adjustment represents an amount that was written off, applied as patient responsibility, or previously paid by another payer. Adjustments can be applied at both the claim level and the service line level.
Payers expect adjustments in a claim to reflect a real dollar amount. A zero amount isn’t valid and will cause the claim to be rejected downstream, which can cause delays.
This new edit – an industry term for an automated validation rule – catches the issue before it reaches the payer. The edit ensures that no claim-level or line-level adjustment in a claim equals zero. If so, the claim fails the edit.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tip
Add the initial treatment date and resubmit the claim.
Dec 1, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when the Payer Claim Control Number (PCCN) is missing when required – or included when it shouldn’t be.
A PCCN is the claim number the payer assigns after they receive and process a claim. It’s the payer’s unique ID for that claim.
You only include a PCCN when you’re replacing or voiding a previous claim. In those cases, payers use it to link the new claim to the original.
If a PCCN is included on a new claim – or missing when you’re replacing or voiding a previous claim – the payer may reject the claim. These edits catch those issues before your claim reaches the payer.
When the PCCN must be included
A claim’s Claim Frequency Code indicates whether it replaces or voids a previous claim. A PCCN is required if the frequency code is:
7– Replacement of Prior Claim8– Void/Cancel of Prior ClaimG– Common Working File (NCH) generated adjustment claimI– Miscellaneous adjustment claimX– Void/Cancel a Prior Abbreviated Encounter SubmissionY– Replacement of prior abbreviated encounter submission
If the PCCN is missing when one of these codes is used, Stedi rejects the claim using a new edit – an industry term for an automated validation rule.
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
When the PCCN must be excluded
If the Claim Frequency Code is not one of the codes above, you should not include a PCCN. If one is present, Stedi rejects the claim using a new edit.
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Dec 1, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when the total claim charge amount is zero and the claim is marked as chargeable.
Most commercial payers do not accept zero-dollar claims. Some scenarios – such as capitated arrangements or encounter submissions – allow them, but standard chargeable claims must have a charge amount greater than $0. Otherwise, the payer will reject the claim, causing delays.
This edit – the industry term for an automated validation rule – catches the issue before the claim reaches the payer.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tip
If the claim was intended for reporting and the total charge should be $0, change the claim’s Claim Identifier to Reporting. If you’re using a JSON claim submission API endpoint, you can do this by changing the top-level claimIdentifier request body property to RP (Reporting).
Dec 1, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims when the total charge amount doesn’t equal the sum of the claim's service line charges.
Payers require these amounts to balance. If they don’t, the payer will reject the claim, which can cause delays. This edit – the industry’s term for an automated validation rule – catches the issue before it reaches the payer.
As part of the edit, we total up the line-level charges and compare them to the claim-level charge. A small rounding tolerance (±$0.01) is allowed. Anything outside that range fails the edit.
The edit applies to all claims, including Coordination of Benefits (COB) claims.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tips
Double-check that the claim-level charge and the sum of the line-level charges match. Most issues come from:
Rounding or formatting errors. For example, using $100.005 instead of $100.00.
Adding, removing, or editing service lines without updating the total.
Dec 1, 2025
Claims
Stedi now rejects secondary and tertiary 837P professional, 837D dental, and 837I institutional claims if the claim’s Coordination of Benefits (COB) amounts don’t balance.
When you submit a secondary or tertiary claim, you must include the payments and adjustments, like patient responsibility or disallowed amounts, from previous payers. These amounts must add up cleanly:
This process is called Coordination of Benefits (COB) balancing.
If the numbers don’t match, the payer may reject the claim to avoid overpayment. This edit – the industry term for an automated validation rule – catches the issue before it reaches the payer.
For more on COB balancing, see our How to balance COB claims guide.
Rejection errors
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Resolution tip
Double-check the payment and adjustment details from the previous payer’s Electric Remittance Advice (ERA), Explanation of Payment (EOP), or Explanation of Benefits (EOB). For help walking through the math, see How to balance COB claims.
Nov 26, 2025
Claims
Stedi now rejects 837P professional, 837D dental, and 837I institutional claims that contain an invalid phone number.
Stedi already fixes common formatting issues for phone numbers in claims. These fixes include:
Removing non-alphanumeric characters, such as spaces, parentheses, or hyphens.
Converting vanity letters, such as those in 1-800-MEDICARE, to numbers
Removing leading country codes, such as
1from 11-digit numbers.
Sometimes, phone numbers still don’t meet phone number validation requirements even after all fixes have been made. Invalid phone numbers will ultimately be rejected by payers, which delays the ultimate adjudication of the claim.
Stedi has introduced a new edit – the industry term for an automated validation rule – to ensure all telephone numbers in a claim are exactly 10 digits after all fixes.
If you submit a claim that fails the edit using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edit using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Nov 26, 2025
Eligibility checks
You can now change how long Stedi retries failed checks in a batch using the new maxRetryHours property of the Batch Eligibility Check API endpoint.
You can set any integer between 8 and 24 hours (inclusive). If you don’t specify a value, the default remains 8 hours.
For example:
Note: You can only set a customer retry window for batch eligibility checks submitted using the Batch Eligibility Check API endpoint.
For more details, see our announcement blog.
Nov 21, 2025
ERAs & transaction enrollment
You can now filter provider records in the List Providers API endpoint by NPI and Tax ID using the providerNpis and providerTaxIds query parameters.
Both parameters expect exact matches and accept multiple values. They can be combined with other filters. The endpoint uses AND logic to return the intersection of all filters.
Example
The following request returns up to 50 provider records whose name contains Dental and whose NPI matches either 1234567890 or 0987654321 and whose tax ID matches either 111223333 or 444556666.
The List Providers endpoint is used to filter provider records used in transaction enrollment requests. For more information, see the transaction enrollment docs.
Nov 21, 2025
ERAs & transaction enrollment
You can now see how long – minutes, hours, days, or weeks – it takes for an enrollment to go from submission to live with a payer in the Stedi Payer Network or the Payers API.
Payer Network
In the Stedi Payer Network, enrollment timeframes are shown in the Payer pane, in the Activation Timeframe field for the transaction type:

Activation Timeframe fields are also listed on the Payer page:

A value of Instant means the enrollment typically goes live within minutes of submission. Other values, like Hours or Days, indicate how long the process usually takes.
Payers API
In Payers API responses, each payer object lists enrollment details, if any, for each transaction type under transactionEnrollmentProcesses. The timeframe field shows the expected enrollment timeline for the transaction type.
For more details, see our announcement blog.
Nov 20, 2025
Claims
Stedi now rejects 837P professional claims and 837I institutional claims with an invalid diagnosis code.
In healthcare claims, diagnosis codes describe what’s wrong with the patient. HIPAA requires that professional and institutional claims only use valid, billable ICD-10-CM codes as diagnosis codes.
What the edits check
Stedi has introduced new edits – the healthcare industry’s term for automated validation rules – to help ensure claims include valid diagnosis codes.
The new edits reject a professional or institutional claim when any diagnosis code is:
Not a valid ICD‑10‑CM code.
For example, if the code is misspelled or doesn’t exist in the official ICD-10-CM code list.A non-billable ICD‑10‑CM code.
Some ICD-10-CM codes are categories. They cover a broad diagnostic grouping rather than a specific condition. For example,E11(Type 2 diabetes mellitus) is a category header.
By themselves, category headers aren’t considered billable codes. They’re not specific enough to describe the exact condition or encounter being billed.
A billable ICD-10-CM code must include both a category and a subcategory, such asE11.9(Type 2 diabetes mellitus without complications).Not valid for the claim’s dates of service.
Updates to the ICD-10-CM code set are published each year. If a claim uses a code that wasn’t valid on the dates of service, Stedi now rejects it.
For example,Z11.52(“Encounter for screening for COVID-19”) became effective on October 1, 2021. A claim with a date of service before that date would be rejected because the code wasn’t valid at the time.
If you submit a claim that fails the edits using Stedi’s claim submission APIs or professional claim form, you’ll get back an error message in real time. If you’re using a JSON API endpoint, the response includes error details in the errors array:
If you submit a claim that fails the edits using SFTP, Stedi will reject the claim with a 277CA claim acknowledgment. The acknowledgment will contain a related claim status category code, claim status code, and error message. You can use the error message to correct and resubmit the claim.
Nov 19, 2025
Claims
You can now upload claim attachments using the professional claims submission form in the Stedi portal.
For claim-level attachments, use Box 19 – Supplemental claim information.

For line-level attachments, use Box 24 – Service lines supplemental information.

You can upload JPG, PDF, PNG, or TIFF files as attachments. To upload an attachment, you must set the Transmission code to EL (EDI).
You must also choose the appropriate Report type for the attachment. For example, if you’re uploading a medical record, you’d select a Report type of M1 – Medical Record Attachment. See Attachment Report Type Codes for a full list.
Note: You can’t add attachments to claims that were already submitted through the portal. To include attachments for those claims, resubmit them with the attachments.
Previously, you could only upload attachments using Stedi’s Create Claim Attachment JSON API endpoint.
For more details, see our announcement blog.
Nov 18, 2025
ERAs & transaction enrollment
You can now download a PDF version of your 835 Electronic Remittance Advice (ERAs) from the Stedi portal.
Each PDF use a layout similar to the CMS Standard Paper Remit (SPR), Medicare’s official paper form for remittance.

For more details, see our announcement blog.
Nov 18, 2025
Eligibility checks
Batch eligibility checks let you run up to 10,000 checks asynchronously using a single request. You can check the progress of those batches with two new API endpoints:
Retrieve Batch Check Status – Shows the overall status of a batch, including counts for completed and in-progress checks.
Retrieve Batch Check Statuses – Shows the status of each individual check in a batch.
For more details, see our announcement blog.
Nov 16, 2025
ERAs & transaction enrollment
You now get back a realistic mock 835 Electronic Remittance Advice (ERA) for claims submitted to Stedi’s test payer.
The mock ERAs mirror the type of electronic remittance you’d receive from payers in production. Each ERA contains the same information as if the test claim were paid in full.
For details, check out our announcement blog.
Nov 12, 2025
Payers
You can now tell which payers support vision coverage using the Stedi Payer Network or the Payers API.
For more details, see our announcement blog.
Nov 10, 2025
Claims
You can now submit claims as X12 EDI in the Stedi portal. Professional, dental, and institutional claims are supported. Previously, you could only submit claims as X12 using our X12 Claims API or SFTP.

For more information, see our announcement blog.
Nov 3, 2025
Claims
Required fields are marked with a red asterisk. For example, in the form, the insured's First and Last name is required.

Nov 3, 2025
Eligibility checks
We’ve redesigned the benefits table for eligibility responses in the Stedi portal to make it faster and easier to read a patient’s benefits.
Benefits are now grouped by health plan. Each plan begins with its general limitations, followed by benefit details. The benefit details are organized by the Service Type Codes (STCs) and procedure codes from the payer’s response.
If present, benefits for STC 30 (Health Benefit Plan Coverage) and STC 35 (Dental Care) – the baseline STCs for medical and dental care – appear first.

The table displays information from the benefitsInformation objects in Stedi’s JSON Eligibility API responses.
Filter benefits
You can filter the table to quickly find benefits for a specific service, procedure, or coverage type – like a deductible or limitation. You can also filter by overage level and whether the benefit applies to in-network or out-of-network services.
For example, you can filter the table to only show individual deductibles for STC 3 (Consultation).

The table displays information from the benefitsInformation objects in Stedi’s JSON Eligibility API responses.
For more information, see our announcement blog.
Nov 3, 2025
Eligibility checks
The Batch Eligibility Check API endpoint now supports up to 10,000 eligibility checks in a single request. Previously, the limit was 1,000 checks per request.
For more information, see our announcement blog.
Oct 30, 2025
Payers
The Stedi Payer Network now displays logos for select payers.
The Payer Network is Stedi's online payer list. The site lets you browse and search Stedi's supported payers for payer IDs, supported transaction types, and transaction enrollment requirements.
Logos make it easier to confirm you’ve found the right payer while browsing or searching.

The payer’s logo also appears on its detail page.

Logos in the Payers API
Stedi’s Payers API now returns the URL for a payer’s logo, when available. You can use the URLs to fetch payer logos for use in your own applications and interfaces.
The logo URL appears in the payer.avatarUrl field of the API response. The field is available for the Search Payer, List Payer, and Retrieve Payer endpoints.
Example:
Oct 23, 2025
Claims
We’ve redesigned the professional claim form in the Stedi portal to make it faster and easier to manually submit 837P professional claims.
The new layout mirrors the CMS-1500 (NUCC) Health Insurance Claim Form, the standard paper form for professional claims in the healthcare industry. If you’ve filled out a CMS-1500 before, the new form will look familiar.

To access the form, sign in to your Stedi account and go to https://portal.stedi.com/app/healthcare/claims/create. You can also open the form from the Stedi portal by going to Claims> Submit claim.
For more details, see our announcement blog.
Oct 6, 2025
Accounts
You can now get free production access to Stedi with the Basic plan.
The Basic plan is our new starter plan for customers who just need to manually process production transactions, such as claims and eligibility checks, in the Stedi portal. It’s great for providers and small practices who are processing a small number of transactions each month.
The Basic plan also allows customers to test API integrations using test API keys. Once they’re finished testing, these customers can upgrade to a Developer plan to send production transactions using real API keys.
For details, see the announcement blog.
Sep 29, 2025
Payers
We’ve expanded the Stedi Agent with two new conversational features:
Payer Finder: Ask questions about payers using conversational AI
Chats: A dedicated page for all your Stedi Agent conversations
You can use these tools to get answers to payer questions faster and easier.
For more information, see the announcement blog.
Sep 24, 2025
ERAs & transaction enrollment
We’re replacing the SUBMITTED transaction enrollment status with two new statuses that show who needs to act next:
STEDI_ACTION_REQUIRED– Stedi needs to take action.PROVIDER_ACTION_REQUIRED– You or the provider need to take action.
The SUBMITTED status is now deprecated. Any existing requests will keep the SUBMITTED status and use the previous status workflow until they're live, canceled, or rejected.
We've also clarified the PROVISIONING status to mean only thing: the request has been submitted to the payer.
These changes make it easier to see which requests need your attention. You can filter by the PROVIDER_ACTION_REQUIRED status in the Stedi portal or List Enrollments endpoint to see which requests require action by you or your provider. For example, using the endpoint:
How enrollment statuses work now

Requests submitted through the Stedi portal or a bulk CSV now start in the STEDI_ACTION_REQUIRED status. If you’re using the Create Enrollment endpoint, you can set the status to STEDI_ACTION_REQUIRED to start processing the enrollment.
Sep 15, 2025
Eligibility checks
The controlNumber request body field is now deprecated in the following JSON API endpoints:
The controlNumber field is now optional. We don't recommend specifying the controlNumber field in requests.
About interchange control numbers
In the underlying X12, an interchange control number is used by payers to detect duplicate transaction submissions. Many payers enforce strict uniqueness rules for interchange control numbers.
When you use Stedi's JSON APIs – like those above – Stedi generates valid, unique interchange control numbers when we translate your JSON API request to X12. We ignore the controlNumber field in the JSON request.
For more information, see our Control numbers in X12 EDI blog.
Sep 10, 2025
Claims
You can now submit 837I institutional claims as X12 EDI using the Institutional Claims X12 API endpoint.
Most Stedi customers submit 837I claims using our JSON-based Institutional Claims endpoint. JSON is familiar and easy to work with. You can build an integration faster.
But if you already work with X12, converting to JSON wastes time. The new endpoint accepts X12 directly.
Previously, X12 submissions of 837I claims required SFTP. With SFTP, you have to wait for files to get errors or validation. With the API, you get instant responses. Development is faster, and debugging is easier.
For complete details, check out the Institutional Claims (837I) Raw X12 API reference.
Sep 2, 2025
Accounts
Stedi integrated accounts and Stedi apps are now available. Together, this new set of capabilities allows end customers of Stedi’s Platform Partners to have Stedi accounts of their own.
Integrated accounts drastically reduce the amount of clearinghouse functionality that partners need to build themselves.
Integrated accounts
Integrated accounts are simplified Stedi accounts that are designed to be friendly to non-technical users. The more complex developer-focused functionality – such as configuring API access and webhooks, and viewing raw JSON payloads – has been removed.
Stedi apps
Integrated accounts can install Stedi apps, which are Stedi’s pre-built integrations to a growing list of third-party RCM, PMS, EHR, and other platforms.
Stedi apps allow providers to quickly connect their Stedi account to these external systems using preconfigured SFTP credentials and API keys.
They can also grant Stedi portal access for external support and implementation teams to assist with setup and ongoing support.
Learn more
See our announcement blog.
Aug 26, 2025
Claims
You can now correct and resubmit claims directly from the transaction detail page of any claim in the Stedi portal.
We’ve also made other UI improvements that make the portal’s Claims section simpler and faster to use. Here’s what’s new:
Streamlined list views and filters on the Transactions and Files pages help you find what you need, fast.
Cleaner detail pages for transactions and files put the most important information front and center.
For more information, see our announcement blog.
Aug 21, 2025
Real-time claim status
You can now run 276/277 real-time claim status checks in the Stedi portal.
You can submit a claim status check using the Stedi portal’s new Create claim status check page. You can access the page by clicking Claims > New claim status in the portal’s nav.

Previously, you could only run these checks using Stedi’s Real-Time Claim Status API.
For more information, check out the announcement blog.
Aug 19, 2025
ERAs & transaction enrollment
You can now download documents for a transaction enrollment request directly from its details page in the Stedi portal. This includes documents signed by Stedi on your behalf if you use delegated signature authority.

For more information, see our documentation.
Aug 19, 2025
Eligibility checks
You can now use the Stedi Agent in sandbox accounts and test mode.
In sandbox accounts and test mode, you run predefined mock eligibility requests that return realistic responses. The Stedi Agent is the Stedi portal’s built-in AI assistant. It helps you recover failed eligibility checks.
Previously, you could only use the Stedi Agent for failed eligibility checks in production. Now, you can try the agent out in sandbox accounts and test mode using a predefined mock check.

For more information, check out the announcement blog.
Aug 18, 2025
ERAs & transaction enrollment
You can now filter results more precisely in the List Enrollments and List Providers API endpoints.
We’ve also updated the Enrollments page and Providers page in the Stedi portal to surface these filters.
List Enrollments endpoint
We’ve added new query parameters to the List Enrollments endpoint. You can use the parameters to filter by:
Partial term:
filterlets you search across multiple fields at once.Status: Filter by one or more enrollment statuses—such as
DRAFT,SUBMITTED,PROVISIONING,LIVE,CANCELED, orREJECTED.Provider details: Filter by NPI (
providerNpis), tax ID (providerTaxIds), or name (providerNames).Payer: Filter by payer IDs (
payerIds).Source: Limit results by how the enrollment was created:
API,UI, orIMPORT.Transaction type: Filter by transaction types, like
eligibilityCheck,claimStatus, orclaimSubmission.Date: Filter enrollments by when they were created (
createdFrom,createdTo) or when their status last changed (statusUpdatedFrom,statusUpdatedTo).Import ID: If an enrollment was created through CSV import, filter by the returned
importId.
Several of these query parameters accept arrays. You can include an array parameter more than once in the URL to filter by multiple values.
List Providers endpoint
The List Providers endpoint now accepts a filter parameter for searching by provider name, NPI, or tax ID. Filtering is case-insensitive and supports partial matches.
Updated filters in the Stedi portal
Alongside API improvements, we’ve updated the Stedi portal to surface these new filters on the Enrollments page and Providers page.
On the Enrollments page:

On the Providers page:

Aug 13, 2025
Eligibility checks
Now available in the Stedi portal, the Stedi Agent brings AI-powered automation to healthcare clearinghouse workflows, beginning with eligibility check recovery.
Use the Stedi Agent to recover failed eligibility checks. If a check fails with a known recoverable error, a Resolve with Stedi Agent option appears next to the related search. The agent runs in Debug view, where you can watch it work – step by step, in real time.

For more information, see our announcement blog.
Aug 11, 2025
Eligibility checks
Stedi now enriches most Blue Cross Blue Shield (BCBS) eligibility responses by automatically including the member’s home payer name and primary payer ID whenever possible.
This info appears in a related benefitsInformation.benefitsRelatedEntities entry in our JSON eligibility responses and in a 2120C or 2120D loop in X12 responses.
For more information, see our announcement blog.
Aug 8, 2025
Accounts
Stedi is now e1 certified by the HITRUST for foundational cybersecurity.
HITRUST e1 Certification demonstrates that Stedi’s healthcare clearinghouse platform is focused on the most critical controls to demonstrate that essential cybersecurity hygiene is in place. The e1 assessment is one of three progressive HITRUST assessments that leverage the HITRUST Framework (HITRUST CSF) to prescribe cyber threat adaptive controls that are appropriate for each assurance type.
Aug 6, 2025
Eligibility checks
You can now run real-time eligibility checks using our CAQH CORE–compliant SOAP API endpoint.
Most Stedi customers use our JSON API for real-time eligibility. But if you're already using CAQH CORE SOAP, this new endpoint is the fastest way to start running eligibility checks with Stedi.
The endpoint supports CAQH CORE Connectivity Rule vC2.2.0. We plan to support CAQH CORE Connectivity Rule vC4.0.0 as industry adoption increases.
For complete details, see our documentation.
Aug 5, 2025
Eligibility checks
Today, Stedi announces the release of its Model Context Protocol (MCP) server.
The MCP server gives AI agents plug-and-play access to Stedi’s Real-Time Eligibility and Search Payers API endpoints, along with built-in guidance for common errors. You can connect your agents without having to write integration code or copy documentation.
For more information, see the announcement blog and our documentation.
Jul 18, 2025
Payers
You can now use the Retrieve Payer API endpoint to get a single payer record by its Stedi payer ID:
The endpoint returns the same payer information as our existing JSON-based Payer API endpoints: payer ID, name, payer ID aliases, transaction support, enrollment requirements, and more. Just for a single payer.
For more information, see the Stedi docs and the announcement blog.
Jul 14, 2025
Accounts
You can now use the Stedi Platform Partners directory to find RCM, EHR, and practice management systems that use Stedi.
Many healthcare companies are looking for modern RCM solutions – and can’t or don’t want to build one themselves. The directory helps you find solutions that are powered by Stedi’s API-first clearinghouse rails.
For more information, see the announcement blog.
Jun 30, 2025
ERAs & transaction enrollment
You can now authorize Stedi to sign enrollment forms for you using delegated signature authority, eliminating over 90% of your team’s enrollment paperwork.
Delegated signature authority is available to all Stedi customers. To get started, reach out to Stedi support.
For more details, see the blog.
Jun 30, 2025
Payers
You can now see whether a payer supports medical or dental transactions using the Payers API and Stedi Payer Network.
Every payer in the network now includes a coverageTypes field in responses from Payers API endpoints. For example, in JSON responses:
If you’re using the Search Payers API endpoint, you can also filter by coverage type. Example:
For more details, see the blog.
Jun 24, 2025
Eligibility checks
You can now run batch 270/271 eligibility checks by uploading a CSV file in the Stedi portal.
Use the new Eligibility check batches page to run batch checks using a bulk CSV:
Submit up to 1,000 checks per file.
Run multiple files at the same time.
Pull results from any batch using the Poll Batch Eligibility Checks API.
Track all batches – CSV or API – in real time, in one place.
For more details, see the blog.
Jun 24, 2025
Payers
You can now use the List Payers CSV API to get a full list of Stedi’s supported payers in CSV format:
The CSV includes the same data as the Stedi Payer Network UI and other JSON-based Payer APIs:
Payer IDs
Transaction support flags
Transaction enrollment requirements, and more.
For complete details, see the List Payers CSV API docs.
Jun 16, 2025
ERAs & transaction enrollment
When the status of a transaction enrollment request changes, Stedi now sends you an automated email.
No setup is needed. These email notifications replace our previous manual notification process.
If an enrollment requires action on your part, we’ll continue to reach out to you via Slack or email with next steps.
For more information, check out our related blog.
Jun 13, 2025
Accounts
CAQH CORE has officially certified Stedi for real-time eligibility checks.
This certification confirms that our 270/271 transactions meet CORE’s strict standards for:
What data a 271 response must include
Standardized error messaging
System uptime and performance under real-world conditions
For more details, see our CORE certification blog.
Jun 5, 2025
ERAs & transaction enrollment
You can now submit transaction enrollments to select payers in a single step.
Just submit an enrollment request using Stedi’s Enrollments API, UI, or a bulk CSV import. We do the rest.
One-click enrollment is available for 850+ payers. Check the Stedi Payer Network or Payer APIs to see which payers are supported.
To learn more, see our full blog.

Jun 4, 2025
ERAs & transaction enrollment
Stedi now has a direct connection to Zelis, a multi-payer provider platform.
Many payers use Zelis as their primary way of delivering 835 Electronic Remittance Advice (ERA) files through clearinghouses to providers.
To receive ERAs from Zelis, providers must set up an account in the Zelis portal. This involves selecting a clearinghouse from a prepopulated list. Previously, providers using Stedi had to select an intermediary clearinghouse in order to receive ERAs.
With Stedi’s new direct Zelis connection, you can now choose Stedi from the list of integrated clearinghouses. Once set up, you’ll automatically receive ERAs from all Zelis-connected payers directly through Stedi.
To submit new enrollment requests, use the Enrollments API, UI, or a bulk CSV import. For Zelis-connected payers, we’ll instruct you to select Stedi as the clearinghouse in Zelis when needed.
If you previously submitted a Stedi enrollment for a Zelis-connected payer, you can log into Zelis and select Stedi as the clearinghouse to transition to Stedi’s direct Zelis connection without any interruption or downtime.
For details, see the blog.
May 28, 2025
ERAs & transaction enrollment
Stedi has partnered with Anatomy, a modern healthcare lockbox and document conversion service, to help you turn paper explanations of benefits (EOBs) into standard 835 Electronic Remittance Advice (ERA) transactions.
Previously, providers receiving paper EOBs had to scan and manually enter payment data, slowing down posting and introducing errors. You can now use Anatomy to handle paper EOBs using your existing digital workflow.
Anatomy accepts paper or PDF EOBs and converts them into 835s. Anatomy then securely sends the 835s to Stedi on your behalf. In Stedi, you can enroll to receive 835s from Anatomy just like you would if they were a payer. You get the ERAs using the 835 ERA Report API or the from-stedi directory of your Stedi SFTP connection. You can use webhooks to get notified when new ERAs are available.
Anatomy is now listed as a supported payer in the Stedi Payer Network. For more details, see the blog.
May 16, 2025
Payers
You can now use the Search Payers API to programmatically search the Stedi Payer Network.
The API lets you search by the payer’s name, payer ID, or payer ID alias. The search supports fuzzy matching, so it returns close matches even if the provided payer name isn’t exact. You can further filter the results by supported transaction types, like dental claims (837D) or eligibility checks (270/271).
The following request searches for the “Blue Cross” payer name and filters for payers that support eligibility checks and real-time claim status.
Visit the Search Payers API docs for complete details.
We’ve also updated the Stedi Payer Network UI to use the new API. You now get consistent search results across the UI and API.

May 2, 2025
Claims
You can now include claim attachments in API-based 837P professional and 837D dental claim submissions.
For more information, see the announcement blog.
Apr 25, 2025
Eligibility checks
You can now request up to 200 results per page when using the pageSize query parameter in the Poll Batch Eligibility Checks API. The previous limit was 10.
With the higher limit, you can retrieve larger sets of eligibility results with fewer API requests.
Visit our batch refresh checks docs for complete details about batch eligibility checks.
Apr 24, 2025
Eligibility checks
The Batch Eligibility Check (270/271) API now supports up to 1,000 eligibility checks per batch. Previously, batches were limited to 500 checks each.
The Batch Eligibility Check (270/271) API lets you submit multiple eligibility checks in a single request, which Stedi processes asynchronously. You can use batch checks to run periodic patient eligibility refreshes before appointments, preventing surprises and billing delays.
Visit our batch refresh checks docs for complete details about batch eligibility checks.
Apr 4, 2025
Claims
The 277 Claim Acknowledgment (277CA) indicates whether a claim was accepted or rejected and (if relevant) the reasons for rejection. You may receive multiple separate 277CAs for each claim you submit to Stedi. Typically, this includes:
277CAs from Stedi reflecting whether the claim was sent to the payer or rejected due to validation issues.
A 277CA from the payer indicating whether the claim was accepted or rejected.
The 277CA Report API now returns additional properties in the transactions.payers array that allow you to quickly determine whether the 277CA was sent by Stedi or the payer. The organizationName property contains the sender's name (such as STEDI INC, or CIGNA), and the entityIdentifierCodeValue property contains either Clearinghouse or Payer.
We also added this information to the top of the 277CA details view in the Stedi portal for easy access.

Visit our claim responses docs for complete details about interpreting and retrieving 277CAs.
Mar 21, 2025
Eligibility checks
Eligibility checks verify a patient's coverage with a specific payer. But what if you don't know the patient's insurance details or you're not sure whether they have coverage at all? Now, you can run an insurance discovery check to find a patient's active coverage using only their demographic data.
You may need to run an insurance discovery check when a patient provides outdated insurance details, doesn’t have their insurance card, or can’t provide insurance details in an urgent care situation. You may also want to use insurance discovery checks to simplify patient onboarding.
Here's how insurance discovery checks work:
Submit a request to the Insurance Discovery API with as much patient demographic information as possible to increase the chances of finding matching coverage. You'll also include information like the provider's NPI and the date of service, similar to an eligibility check.
Stedi uses the demographic information you provide to determine if the patient has active coverage with one or more payers. This process involves submitting real-time eligibility checks to supported payers to find a match.
When the insurance discovery check is complete, Stedi returns an array of potential active coverages along with subscriber details and complete benefits information.
There is no cost for limited insurance discovery checks while the API is in beta. If you are interested in pricing when the product is generally available, please contact us.
Visit our Insurance Discovery docs for complete instructions, example requests and responses, and more.
Mar 19, 2025
ERAs & transaction enrollment
The 835 ERA Report API retrieves 835 Electronic Remittance Advice (ERA) transactions from Stedi in developer-friendly JSON. The ERA data now contains full Claim Adjustment Reason Code (CARC) and Remittance Advice Remark Code (RARC) descriptions, making it easier to interpret the payer’s response.
CARC codes describe why a claim or service line was paid differently than it was billed. Now, adjustments objects for both the claim and specific service lines contain an adjustmentReason property with the full code description. The following example shows the adjustmentReason1 property within the transactions.detailInfo.paymentInfo.serviceLines.serviceAdjustments object.
RARC codes provide additional explanations for adjustments or convey information about remittance processing. Now, transactions.detailInfo.paymentInfo.claimAdjustments.serviceLines.healthCareCheckRemarkCodes objects contain an additional remark property with the full code description.
Mar 6, 2025
Claims
This new endpoint allows you to use a Stedi business identifier (the claim’s correlation ID) to retrieve the CMS-1500 PDF for submitted 837 professional claims.
Call the endpoint with the business identifier as a query parameter for the claim form PDFs you want to retrieve. The business identifier should be the claim’s correlation ID. You can find this value in the
claimReference.correlationIdproperty in the synchronous responses from the Professional Claims and Professional Claims Raw X12 endpoints.Stedi returns an array of PDFs for all claims with the specified business identifier value. The PDFs are returned as a base64 encoded string.
Decode the base64 string and save it to a file with a .pdf extension.
Visit the CMS-1500 PDF: Business Identifier API docs for complete details.
Mar 4, 2025
Eligibility checks
Test mode provides a separate test environment where you can simulate transactions in your Stedi account without PHI/PII and without sending any data to payers.
In test mode, you can submit mock real-time eligibility checks and Stedi sends back a realistic benefits response so you know what kinds of data to expect in production. You can send mock requests for a variety of well-known payers, including:
Aetna
Cigna
UnitedHealthcare
National Centers for Medicare & Medicaid Services (CMS)
Many more - Visit Eligibility mock requests for a complete list
After you submit a mock eligibility check, you can review all of the request and response details in the Stedi portal. This includes a user-friendly benefits view designed to help you quickly understand the patient’s active coverage and payment responsibilities.
To access test mode in your account, toggle Test mode to ON. Visit the test mode docs for more details.
Feb 28, 2025
Claims
You can use Stedi’s fully-managed SFTP server to submit claims to payers and retrieve claim responses. Stedi SFTP is a great option if you have an existing system that generates X12 EDI files and you want to send them through the Stedi clearinghouse without an API integration.
Here’s how SFTP claims processing works:
Create both test and production SFTP users through the Healthcare page in Account settings. Test users can only send claims to Stedi’s test clearinghouse, which helps ensure you never accidentally send test claims to payers while you’re getting up and running.
Connect to Stedi's server and drop compliant X12 EDI claim files into the
to-stedidirectory.Stedi automatically validates the claim data. If there are no errors, Stedi routes your claims to the test or production clearinghouse.
Stedi places claim responses - 277 Claim Acknowledgments and 835 Electronic Remittance Advice (ERAs) - into the
from-stedidirectory in X12 EDI format.You retrieve claim responses from the SFTP server at your preferred cadence.
You can also configure Stedi webhooks to send claim processing events to your endpoint. This allows you to monitor for processing issues, confirm successful claim submissions, and get notified when new payer responses are available.
Visit the SFTP claim submission docs for complete details.
Feb 28, 2025
ERAs & transaction enrollment
Developers and operations teams can now submit transaction enrollments to payers using bulk CSV import functionality. This allows you to submit hundreds of enrollment requests to Stedi in minutes.
Here’s how it works:
Go to the Bulk imports page and click New bulk import.
Download the CSV template with the required fields. The upload page contains detailed formatting instructions.
Complete and upload the CSV file containing enrollment information—one row equals one enrollment request for a specific transaction to a payer.
Stedi checks the file for errors and notifies you of any issues. You can fix the errors and re-upload the file as many times as needed.
Once you execute the import, Stedi automatically creates provider records and enrollment requests.
When the import is complete, you can download a report that shows the status of each row in the CSV file to ensure all your enrollment requests were submitted successfully. You can also track the status of each new enrollment request through the Enrollments page.
The Stedi team will contact you with any additional information required for the enrollment and will let you know when it is live.
Visit the Stedi Payer Network to find out if a payer requires enrollment for a particular transaction type.
Feb 21, 2025
Eligibility checks
A Medicare Beneficiary Identifier (MBI) is a unique, randomly-generated identifier assigned to individuals enrolled in Medicare. You must include the patient’s MBI in every eligibility check you submit to the Centers for Medicare and Medicaid Services (payer ID: CMS). When patients don’t know their MBI, you can use Stedi's eligibility check APIs to perform an MBI lookup using their Social Security Number (SSN) instead.
To perform an MBI lookup:
Construct an eligibility check request with the patient’s first name, last name, date of birth, and Social Security Number (SSN).
Set the
tradingPartnerServiceIdtoMBILU. This is a special payer ID that tells Stedi to perform an MBI lookup for the patient in addition to a standard eligibility check.Stedi returns a complete benefits response from CMS with the patient's MBI in the
subscriberobject for future reference.
Visit our Medicare Beneficiary Identifier (MBI) lookup docs for complete details.
Feb 14, 2025
Claims
The view for 277CA Claim Status transactions includes the following improvements:
Key claim details, including the patient account number and the claim value, are at the top for easy access.
Claim Status codes are displayed with clear descriptions, and processing issues are flagged to help you quickly catch errors and understand what went wrong.
Related transactions, including the original claim, are identified and linked.
The transaction’s raw input and output are available for review and download.
To check out the updated view, click any 277CA Claim Status transaction listed on the Stedi Transactions page.

Feb 5, 2025
Eligibility checks
You can now submit coordination of benefits (COB) checks through the Coordination of Benefits Check API for any of Stedi’s supported COB payers.
You submit COB checks programmatically in developer-friendly JSON. The information required is similar to a standard eligibility check – the patient's first name, last name, DOB, and either member ID or SSN.
Stedi synchronously returns summary information about each of the patient’s active health plans and whether there is coverage overlap. When there is coverage overlap, Stedi returns the responsibility sequence number for each payer (such as primary or secondary, if that can be determined).
Visit the Coordination of Benefits Check API documentation for full details, test requests and responses, and more.
Jan 9, 2025
Eligibility checks
You can now create test API Keys for development and integration testing.
Test API keys allow you to conduct integration testing on specific Stedi APIs without sending data to partners or processing PHI or PII. You can generate production and test API keys from the API Keys page in your Stedi account.
At launch, test API keys support hitting the Real-Time Eligibility Check API with the mock requests we have available. We will add support for other APIs in the near future. All mock requests sent with a test API key are free for testing purposes and won’t incur charges in your Stedi account.
Jan 7, 2025
Eligibility checks
When a patient is covered by more than one health plan, you need to know which plan is primarily responsible for paying claims (coordination of benefits). You can now submit coordination of benefits (COB) checks in the Stedi UI to determine:
If a patient is covered by more than one health plan
Whether coverage overlap requires coordination of benefits
Each payer’s responsibility for payment (primacy) in coordination of benefits scenarios

For each COB check, Stedi searches a national database of eligibility data from state and commercial payers. This database has 245+ million patient coverage records from 45+ health plans, ASOs, TPAs, and others, including participation from the vast majority of national commercial health plans. Data is updated weekly to ensure accuracy.
The response includes information about the patient’s active health plans, whether coordination of benefits is required, and the responsibility sequence number for each payer if available (such as primary or secondary).
To help reduce claim denials, we recommend coordination of benefits checks for all new patients with coverage through one of Stedi’s supported COB payers. Visit the Payer Network for a complete list.
Dec 17, 2024
ERAs & transaction enrollment
Developers and operations teams can now submit enrollments one at a time or in batches through Stedi’s user-friendly Enrollments dashboard or modern Transaction Enrollment API.
Both submission methods follow the same streamlined process:
Add provider: You add a new provider record with the information required for enrollment, including the provider's name, tax ID, NPI, and contact information.
Submit transaction enrollment request: You submit requests to enroll the provider with required payers, one for each transaction type. For example, you’d submit three separate requests to enroll a provider for 837P (professional) claims, 270 real-time eligibility checks, and 835 ERAs (claim payments). You can save requests in
DRAFTstatus until you're ready to submit them to Stedi. Once you submit an enrollment request, its status is set toSUBMITTED, and it enters Stedi’s queue for processing.Provisioning: Stedi begins the enrollment process with the payer and sets the enrollment status to
PROVISIONING. Our team leaves clear instructions about what to do next, if required, and provides hands-on help as needed with additional steps.Enrollment is Live: Once the enrollment is approved, the enrollment status is set to
LIVE, and the provider can start exchanging the enrolled transactions with the payer.
You can find out if a payer requires enrollment for a particular transaction type in the Stedi Payer Network.
Dec 3, 2024
Claims
You can use Stedi’s new Dental Claims API to send 837D (dental) claims through the Stedi Clearinghouse:
Dental Claims: Submit your claim in user-friendly JSON. Stedi translates your request to the X12 EDI 837D format and sends it to the payer.
Dental Claims Raw X12: Submit your claim in X12 EDI format. This is ideal if you have an existing system that generates X12 EDI files and you want to send them through Stedi’s API.
Both endpoints return a response from Stedi in JSON format containing information about the claim you submitted and whether the submission was successful. Later, the payer will respond with Claim Acknowledgments (277CA) and the ERA (835), which you can retrieve using Stedi’s APIs.
Visit the Stedi Payer Network to find every supported payer for dental claims.
Nov 26, 2024
Eligibility checks
You can now use Stedi’s Batch Eligibility Check API to submit multiple eligibility checks in a single request for Stedi to process asynchronously.
You can submit up to 500 individual eligibility checks within a single batch, and you can submit as many batches as you need to process. After you’ve submitted a batch of eligibility checks, you can use the Poll Batch Eligibility Checks endpoint to retrieve the results.
We recommend using this new API to perform batches of eligibility checks, such as during periodic refreshes for a patient population or when running weekly eligibility checks for upcoming appointments. Asynchronous batch checks don’t count toward your Stedi account concurrency budget, allowing you to stage thousands of batch checks while continuing to send real-time eligibility checks in parallel.
Nov 20, 2024
Claims
You can use the new Institutional Claims API to send 837I institutional claims through the Stedi clearinghouse.
Call the endpoint with a JSON payload.
Stedi translates your request to the X12 EDI 837I format and sends it to the payer.
The endpoint returns a response from Stedi in JSON format containing information about the claim you submitted and whether the submission was successful.
Later, the payer will respond with Claim Acknowledgments (277CA) and the ERA (835), which you can retrieve using Stedi’s APIs.
Oct 7, 2024
Eligibility checks
You can now submit five new mock requests for dental benefits to the Eligibility Check endpoint, and Stedi returns mock eligibility responses you can use for testing. To send a mock request, you need a Stedi API key for authentication, and you must set the stedi-test header to true.
Try it now for Ameritas, Anthem Blue Cross Blue Shield of CA, Cigna, Metlife, and UnitedHealthcare.
Oct 7, 2024
Payers
Use the new List Payers API to programmatically retrieve information about thousands of supported payers in our Payer Network.
The following Blue Cross Blue Shield of North Carolina response example shows that real-time eligibility checks, real-time claim status requests, and professional claims are supported for this payer. The response also indicates that payer enrollment is required for 835 ERAs (claim remittances).
Sep 3, 2024
Claims
We adapted the National Uniform Claim Committee (NUCC) 1500 Claim Form into a user-friendly digital form you can use to submit claims manually.
Our in-app form validates provider NPIs and other key information to reduce errors and payer rejections. You can also review a live preview of the autogenerated JSON payload for our Professional Claims API to understand how the form relates to the request structure.
To submit a manual claim, visit the Create manual claim page in the Stedi app.
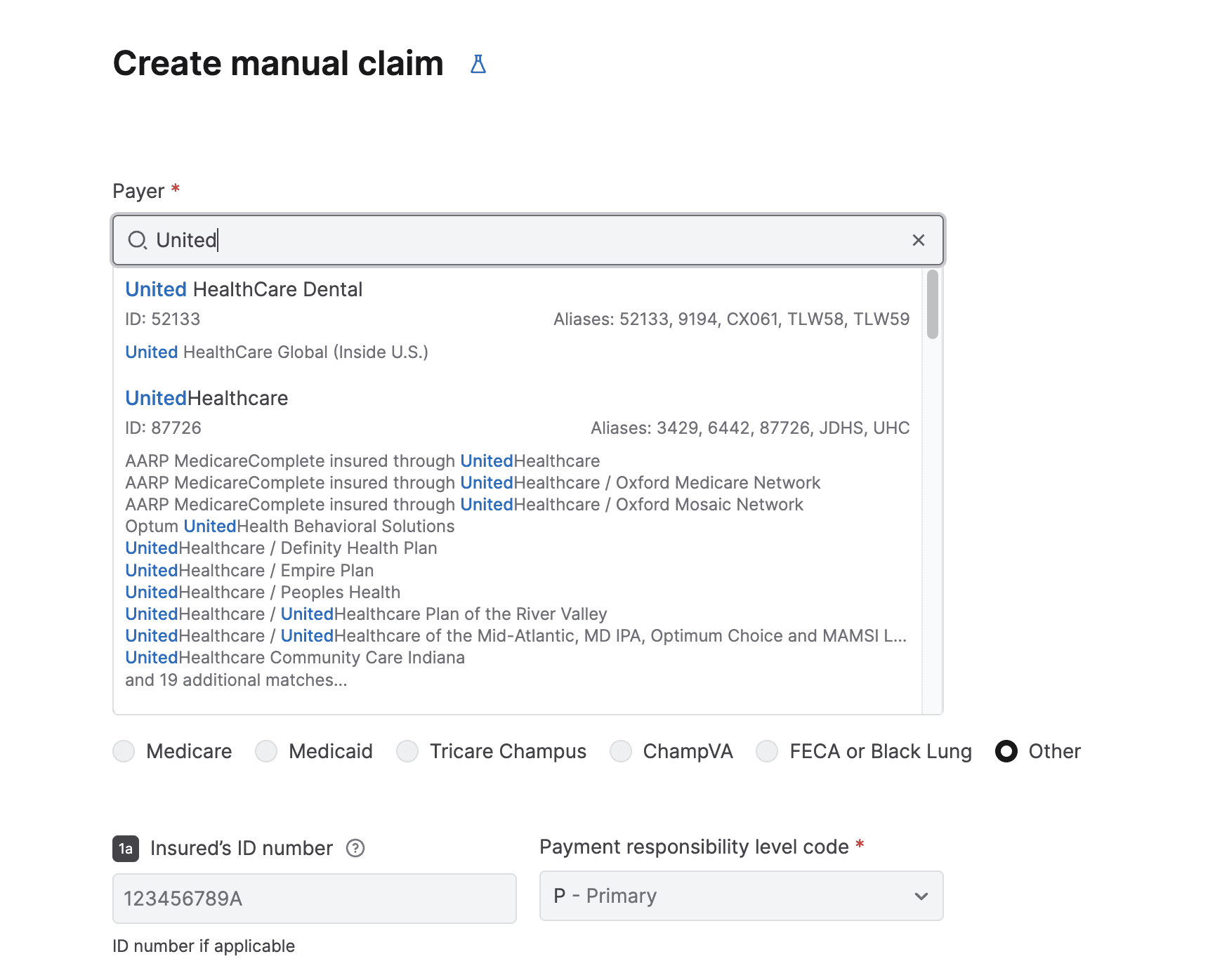
Aug 21, 2024
Claims
You can now use the CMS-1500 Claim Form PDF API to programmatically retrieve auto-generated claim forms for submitted 837 professional claims. All you need is an API Key for authentication and Stedi’s transaction ID for the processed claim.
You can use the API to make auto-generated claim form PDFs available for download within an EHR, practice management, or revenue cycle system. You can also automate retrieving them for internal use, such as record-keeping, mailing and faxing claims to payers, or reviewing claim information in a familiar format.
Aug 15, 2024
EDI platform
Stedi can now automatically generate and deliver negative TA1s for inbound transactions. TA1 Interchange Acknowledgments indicate receipt of an interchange and identify any errors in the interchange’s envelope (ISA and IEA) information.
Stedi can generate two types of negative TA1s:
Accepted with errors: TA1s with code
EinTA104indicate that the interchange was accepted with errors. Stedi proceeds with processing the transaction and creates a record in the Stedi appRejected because of errors: TA1s with code
RinTA104indicate that the interchange was rejected and that Stedi won’t continue processing the transaction.
You can enable automatic TA1s in each partnership’s Acknowledgments settings. Visit the Acknowledgments documentation for complete details.
Jul 29, 2024
Payers
You can use the new List Payers API to programmatically retrieve information about every supported payer in our Payer Network. The response includes:
The payer’s name, payer ID, payer ID aliases, and alternative names.
Whether the following transactions are supported: real-time eligibility checks, professional claims, real-time claim status requests, and ERAs (claim payments).
Whether payer enrollment is required for each transaction type.
Jul 24, 2024
EDI platform
Stedi can now automatically generate positive TA1s for inbound transactions and deliver them to your trading partners.
TA1 Interchange Acknowledgments indicate receipt of an interchange and identify any errors in the interchange’s envelope (`ISA` and `IEA`) information. Positive TA1s contain code `A` in the `TA104` element to indicate you received the interchange successfully, and it contains no errors.
Enable automatic TA1s for each partnership in the Acknowledgments settings. You can send TA1s for every inbound file or only when your trading partner requests them. Visit the Acknowledgments documentation for complete details.

Jul 17, 2024
Claims
The transaction details page has the following improvements:
For 837P (professional) claims, Stedi automatically puts key details, including subscriber information and the claim value, at the top for easy access. You can also instantly download a PDF of the autogenerated 1500 Claim Form.
Transactions with a common business identifier are clearly identified and linked, so you can easily move between related transactions.
The transaction’s raw input and output are available for review and download.
Multiple other UX updates to make the transaction’s data easier to understand and digest.
You can review this information by clicking any transaction on the Transactions page in the Stedi app.

Jul 8, 2024
ERAs & transaction enrollment
You can now use the following APIs to retrieve payer responses in JSON format:
Get 277 Report: Retrieve processed 277 Claim Acknowledgments
Get 835 Report: Retrieve processed 835 Electronic Remittance Advice (ERA) transactions
You can either poll or listen for event-driven webhooks to discover new payer responses. Then, you can call the Report APIs to retrieve the processed responses from Stedi. For convenience, Stedi returns 277s and 835s in the same JSON format as the Change Healthcare (CHC) Convert Reports APIs.
Jul 7, 2024
Claims
For every claim you submit through our Professional Claims APIs, Stedi now automatically generates a complete 1500 Claim Form. You can download these PDF claim forms from the transaction detail page for that claim in the Stedi app.
This feature is useful when you need to export claim forms for record-keeping purposes, physically mail a claim to a payer, or review specific claim information in a familiar format.

Jun 28, 2024
EDI platform
You can now review a mapping’s version history, compare older versions with the current, and instantly roll back to any published version. This functionality helps you better understand the updates made in each version and debug issues in production mappings.
To review a mapping’s version history, go to the mapping, open the Actions menu, and select Version history. You can choose to publish an older version or compare it with the current version in production. Comparing highlights every difference between the old and current versions to show you what has been added or deleted.

Jun 27, 2024
Eligibility checks
The following APIs are now available for customers who want to send raw X12 EDI to payers. These APIs are ideal for companies that generate X12 EDI internally and want to use Stedi to validate and deliver these transactions to payers.
Eligibility Check Raw X12: Send raw X12 EDI 270 Eligibility Benefit Inquiry transactions and receive the payer’s raw X12 EDI 271 Eligibility, Coverage, or Benefit Information in the response - all in real time.
Professional Claims Raw X12: Send raw X12 EDI 837P (professional) Health Care Claims to payers.
Claim Status Raw X12: Send raw X12 EDI 276 Claim Status requests and receive the payer’s raw X12 EDI 277 Status Request Response - all in real time.
Jun 27, 2024
Eligibility checks
You can now send eligibility checks to more than 200 dental payers through Stedi’s growing Payer Network. New dental payers include Guardian, Delta Dental, UHC Dental, Anthem Blue Cross Blue Shield, Pacificare Dental & Vision Plan, Aetna Dental, Cigna Dental, and more.
Search the Payer Network to instantly find the payer ID for any payer and use it to start sending real-time eligibility checks through Stedi’s Eligibility Check API.
Jun 26, 2024
Payers
We redesigned the Stedi Payer Network to make it more comprehensive and user friendly. Improvements include:
Enhanced searching and filtering capabilities so you can instantly find the payers you need for your use case.
Alternative payer names to help you identify payers using the name most familiar to your organization. For example, “Eaton Benefits Ohio” is an alternative associated with “Cigna”—searching for either name returns the same payer within the database.
UX improvements, including clearly showing all of the transaction types supported for each payer as well as the payer ID and any payer ID aliases.
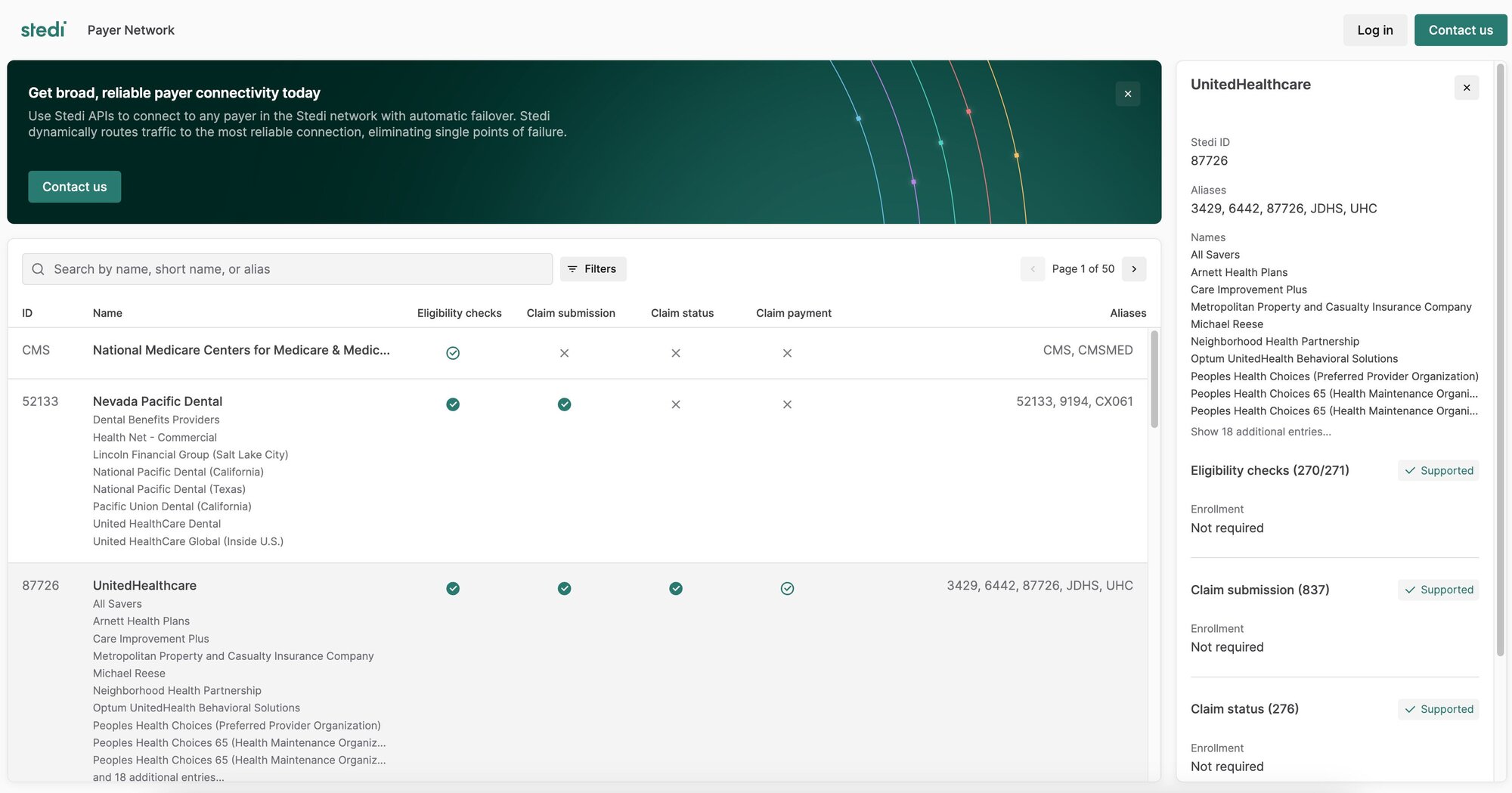
Jun 12, 2024
EDI platform
The Mappings UI now autosaves your changes and stages them for publishing. When you’re ready, you can promote changes to production by clicking Publish changes. You can also discard changes to revert back to the previously published version.

May 30, 2024
Eligibility checks
You can now submit mock requests to the Eligibility Check endpoint, and Stedi returns mock eligibility responses you can use for testing. To send a mock request, you need a Stedi API key for authentication, and you must set the stedi-test header to true.
May 30, 2024
EDI platform
The List Transactions and Poll Transactions APIs now return business identifiers for each transaction.
Business identifiers are values you can use to correlate a transaction with related transactions or other data in your business system. For example, Stedi automatically marks the purchase order number (PRF01) as a business identifier for 850 Purchase Orders.
The following example shows a truncated API response containing the new businessIdentifiers object.

May 15, 2024
EDI platform
You can now set custom filenames for generated EDI files within outbound transaction settings.
By default, Stedi autogenerates a unique name for outbound files using a UUID. To specify a custom filename, open Advanced settings in the outbound transaction setting and enter a JSONata expression into the Filename expression field.
You can use & (Concatenation) or $millis in the expression to generate a unique name based on the processing timestamp. For example, the expression “EDI850-” & $millis() results in filenames like EDI850-5182341242.

Apr 22, 2024
EDI platform
You can now lock mappings in your account to prevent accidental changes or deletions. Any user in your Stedi account can lock a mapping, but only an account admin can unlock it.
You can lock the entire mapping or just the mapping definition. When you lock the mapping definition only, you can add or edit lookup tables, but you cannot edit the mapping source schema, target schema, or mapping expressions.
To lock a mapping, open it, click the ...(ellipses) menu next to its name, and select Lock settings.

Apr 12, 2024
EDI platform
We released the following EDI platform features:
You can now lock guides in your account to prevent accidental changes or deletions. Any user in your Stedi account can lock a guide, but only an account admin can unlock them. To lock a guide, go to the Actions menu and select Lock.

When configuring an outbound test file, you can now review the EDI that Stedi will generate from your JSON test data. To generate an outbound test file, go to the Files page, open the Create file menu, and select Test outbound.

Apr 12, 2024
EDI platform
The new Map Transaction Output endpoint applies a Stedi mapping to a previously processed inbound transaction and returns the fully mapped output.
You can use the endpoint to retrieve processed transaction data asynchronously and ingest it into your business system. This approach can be helpful when the mapped output is too large for Stedi to deliver through a Destination webhook.
Apr 12, 2024
Payers
Introducing the Stedi Payer Network - a comprehensive list of every payer Stedi supports for eligibility checks, claim submission, and claim status checks. You can search by the payer’s name or payer ID alias to retrieve their payer ID, learn which Stedi APIs are supported, and determine whether or not the payer requires provider enrollment.

Apr 12, 2024
Eligibility checks
The Eligibility Check API now returns detailed AAA error messages that specify why the payer rejected the transaction and any recommended follow-up actions. Stedi includes this information in the aaaErrors object in the response JSON.
The following example shows an error at the subscriber level:

Visit our eligibility check troubleshooting docs for a complete list of all possible error types and resolution steps.
Apr 12, 2024
Claims
Our Professional Claims API now automatically replaces non-Latin characters with their Latin equivalents.
Claim submissions with non-conforming characters are a common cause of 999 rejections from the payer. The new autocorrect feature will help reduce these types of errors and the (often significant) time and manual work it takes to fix them.
Apr 12, 2024
Eligibility checks
When you perform a manual eligibility check through the Stedi app, you can now review a more user-friendly 271 Eligibility, Coverage, or Benefit Information response organized by coverage type and level. Click a row to review more details about the benefit type, including the Service Type Code (STC) and the raw JSON response data.
Submitting a manual eligibility check can be useful for testing and when you need to do a one-time eligibility check. Learn more about eligibility checks in our docs.

Apr 2, 2024
Real-time claim status
Stedi’s Claim Status endpoint directly replaces the Change Healthcare (CHC) Claim Status API. You can use it to check the status of an existing claim.
Call Stedi’s endpoint with a JSON payload in the CHC 276 Claim Status format.
Stedi automatically maps CHC payer IDs to our IDs.
Stedi translates the JSON to the X12 EDI 276 format and delivers it to the payer or peer clearinghouse.
The endpoint returns a synchronous 277 response in the CHC Claim Status response JSON format.
Visit the Claim Status API docs for more information.
Mar 28, 2024
Eligibility checks
From the Eligibility menu in the Stedi app, you can now perform the following actions:
Submit manual eligibility checks and review the full 271 JSON response. This feature is useful for testing and for operations teams who need to do one-off checks.

Review errors for every eligibility check you send through the Stedi API and the app. You can filter by payer or timeframe (last hour, last day, or last week) and view details about each error code.

Mar 27, 2024
EDI platform
The Stedi app now displays Destination webhook delivery attempts to help with testing and debugging. This page includes metadata about the delivery attempt, including the destination, the time of the attempted delivery, and detailed logs about each delivery stage.
To review delivery attempts, click a processed file or transaction, click any event to view its details page, and then go to the Destination attempts tab.

Mar 19, 2024
EDI platform
Stedi can now validate and translate inbound EDI files containing multiple interchanges. The interchanges in the file must have the same partnership and direction (matching sender and receiver IDs).
Learn more about inbound file processing.

Mar 19, 2024
Accounts
You can now require all users to enable Multi-Factor Authentication (MFA) before accessing your Stedi account. To enforce MFA for all users:
Click the account name.
Select Account settings and toggle MFA to ON.
The next time each user logs into the account, Stedi prompts them to set up their MFA token. Once you enable MFA for a Stedi account, it cannot be disabled.

Mar 19, 2024
EDI platform
The following improvements make it easier to build and update Stedi mappings.
You can now view more context about Stedi guide segments and elements when you hover over them, allowing you to understand which part of the guide you are mapping more easily. This is especially helpful for large guides, including many X12 HIPAA guides, that repeat the same loop or segment in multiple locations.

You can now search within a mapping’s source or target fields for a specific text string and jump to each matching value. For example, you might search for the name of a specific segment or element.

Mar 19, 2024
EDI platform
Connections and Destination webhooks now apply an automatic filter that displays the last hour of logs by default. You can remove or adjust this time filter as needed.

Mar 19, 2024
EDI platform
It’s now easier to build custom healthcare guides that conform to X12 HIPAA specifications. When creating a new guide, set the X12 Release to 5010 HIPAA. Stedi automatically preloads every HIPAA transaction set from the Stedi Network for you to choose as a base for customization.
Stedi guides are machine-readable versions of the EDI requirements trading partners typically provide as PDF, CSV, or Word documents. You can use Stedi’s guide builder to customize any X12 HIPAA transaction for your EDI integration. Then, you can make your guides public to share them with trading partners as user-friendly, interactive web pages.

Feb 29, 2024
EDI platform
The Generate EDI API now supports idempotent requests.
When you send a request to the Generate EDI API, you can include an idempotency key to prevent sending duplicate data to your trading partners. In the event of network errors or other intermittent failures, you can safely retry requests with the same idempotency key as many times as necessary within 24 hours after making the first request. Learn more.
Feb 23, 2024
EDI platform
We made the following improvements to the Stedi app:
Execution metadata: You can now view file execution metadata, which includes the X12 Interchange and Functional Group values, along with other processing information. To view a file’s execution metadata, go to the Files page, click the file you want to view, and select Raw Metadata in the Results tab.

Event retries: You can now retrigger individual events from both the transaction details page and the file details page.
AS2 certificate validation: Stedi now gives you immediate feedback about errors in your local and partner signing and encryption certificates. For example, you will now receive an error when your certificate is improperly formatted, when a certificate doesn’t validate against a certificate chain, when a public and private key pair don’t match, and more.
Feb 23, 2024
EDI platform
You can now find the following X12 HIPAA guides in the Stedi Network:
Health Care Services Review Information - Acknowledgment (X216)
Health Care Services Review Information - Notification (X216)
The Stedi Network is a free and open catalog of Stedi guides for hundreds of popular trading partners. You can import any X12 HIPAA guide into your account for free and use it in your EDI integration.
Request guides: If you don’t see your partner’s guides in the Stedi Network, submit a request, and we’ll build the guides you need for free in 1-2 business days.
Feb 21, 2024
EDI platform
We updated the authorization scheme in our API to better align with OpenAPI specifications.
The Authorization header no longer requires the Key prefix. Instead, you should now provide API keys directly (Authorization ${STEDI_API_KEY}). This change aligns with the OpenAPI standard and allows for out-of-the-box compatibility with OpenAPI tools and services.
Previously, our APIs required API keys to be passed with a Key prefix (Authorization: Key ${STEDI_API_KEY}), which required manual setup to work with OpenAPI. We will continue to support the previous format for backward compatibility, but we encourage you to adopt the new format to leverage the benefits of OpenAPI compliance.
Feb 20, 2024
EDI platform
You can now read and write EDI for X12 release 008050, the latest version approved in December 2023 and released in February 2024. Stedi now supports every release from 002001 (released in 1987) to present.
The 008050 release is supported throughout the entire Stedi platform. You can review every 008050 transaction set in EDI Reference, create PDF and machine-readable 008050 Stedi guides for your trading partners and EDI integrations, and process live 008050 transactions instantly.
Feb 19, 2024
EDI platform
Stedi Destinations now pre-fills the grant_type header for OAuth 2.0.
When you create or edit a Stedi Destination with OAuth 2.0 configured, the Header parameter grant_type is now pre-populated with client_credentials. This is the most common grant type used when the client is acting on its own behalf. You can change this value in the Advanced menu if you need to use a different grant type.
This change helps ensure that your OAuth 2.0 connections are set up correctly and securely, without extra manual configuration.
For more details on the OAuth 2.0 protocol, visit RFC 6749 section 4.4, which outlines the protocol for the client credentials grant.
Feb 8, 2024
EDI platform
You can now set a custom Interchange Version Control Number Code (ISA-12) for generated EDI files.
When you call the Generate EDI API, the outbound transaction setting ID you provide dictates which Stedi Guide will be used for validation and translation. By default, Stedi sets ISA-12 to be the X12 release number of the associated guide. However, some trading partners may require that you specify a different release for the transaction and the ISA envelope – for example, you might send a transaction from X12 release 003020 inside an ISA envelope with an Interchange Version Control Number Code of 00401.
Visit the Generate EDI docs for complete details about ISA and GS overrides.
Feb 1, 2024
EDI platform
You can now use Stedi to read and write any transaction set from all releases in the 1980s-era X12 Version 2:
002001| Release year: 1987002002| Release year: 1988002003| Release year: 1988002040| Release year: 1989
With this update, Stedi now has complete coverage of all transaction sets across all releases from X12 002001 to X12 008040.
Stedi also now supports custom GS-08 Industry Identifier Codes for all X12 releases when reading and writing EDI.
Industry Identifier Codes are the 1-6 characters appended to the end of a release in the GS-08 element – for example, 005010UCS and 004010VICS or 005010X279A1 in the X12 HIPAA standard. You can now define your own custom identifier for any transaction set as needed. Custom identifiers are helpful when trading with automotive OEMs such as Ford (which uses 002002FORD) and Chrysler (which uses 002040CHRY).
Jan 29, 2024
EDI platform
We consolidated the top navigation bar to make the Stedi app easier to use and understand.
The top navigation is now organized into three sections:
Files: Review, sort, filter, and inspect every file flowing through Stedi. This page was previously called File executions.
Transactions: Review, sort, filter, and inspect every EDI transaction flowing through Stedi.
Setup: Access all the tools and configurations required to onboard and manage trading partners. This menu includes Trading partners, Guides, Destinations, EDI settings, and Mappings (if applicable).
We also consolidated documentation and resources into a single menu and co-located key account admin pages, such as Account settings, under the account selection menu.

Jan 25, 2024
EDI platform
Stedi stores metadata about each successful file execution, such as the processing timestamp and X12 Interchange and Functional Group values. You can now retrieve this metadata through the following methods:
The
file.processed.v2event includes a metadata artifact with a document download URL you can use to fetch the execution metadata.The Get Execution Metadata API returns a document download URL you can use to fetch the execution metadata.
Jan 25, 2024
EDI platform
You can now retrigger events for successfully processed files. This feature makes it easier to test your end-to-end integration – for example, triggering webhooks – without continually reprocessing the same files.
To retry an event:
Go to the Files page.
Click the name of the processed file.
Go to the Events tab.
Click the ellipses (...) next to an event and select Retry.

Jan 22, 2024
EDI platform
The HIPAA 999 Implementation Acknowledgment is now available in the Stedi Network’s collection of X12 HIPAA guides.
The Stedi Network is a free and open catalog of Stedi guides for hundreds of popular trading partners. Stedi guides are a machine-readable format for EDI requirements that Stedi uses to automatically validate, translate, and generate EDI according to trading partner’s requirements.
You can import the 999 into your account for free and add it to transaction settings for your EDI integration.
Request guides: If you don’t see your partner’s guides in the Stedi Network, submit a request, and we’ll build the guides you need for free in 1-2 business days.
Jan 18, 2024
EDI platform
To make debugging easier, you can now set the log level for each Destination webhook. Destination webhooks allow you to send transaction data and events from Stedi to any external API.
You can edit the webhook to switch between the following log levels at any time:
OFF- no logsERROR- errors onlyINFO- errors and select execution steps, such as successful deliveriesTRACE- all execution steps
To review a webhook’s logs, click its name and then go to the Logs tab.
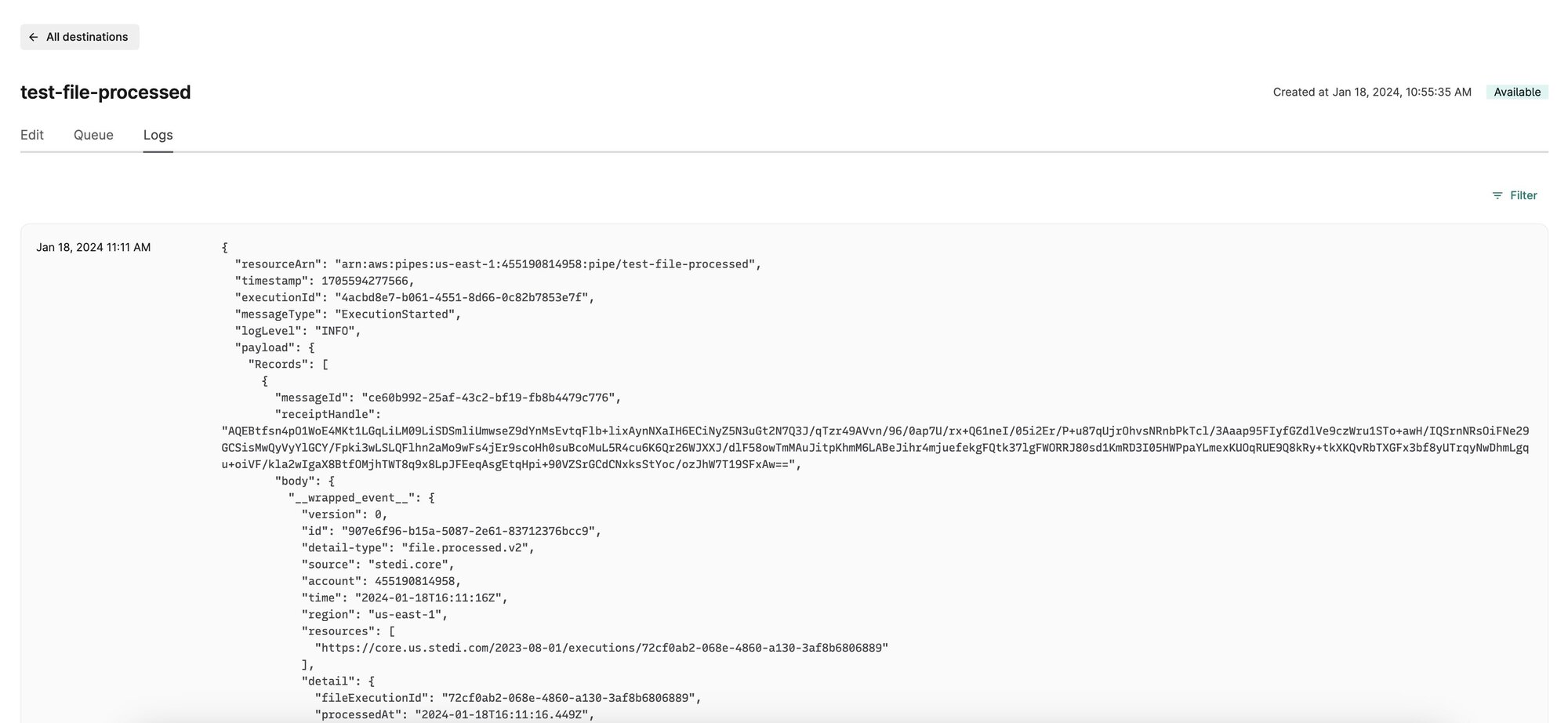
Jan 12, 2024
EDI platform
When building a Stedi mapping for reading EDI, you can now switch between the sample files attached to the source guide. Sample files typically represent the use cases when you could receive that transaction set from your trading partner. For example, the X12 HIPAA 834 Benefit Enrollment and Maintenance guide includes samples for adding subscriber coverage, canceling a dependent, changing subscriber information, and more.
As you switch between samples, Mappings dynamically updates the source JSON shape and the expected mapping results, so you can ensure your mapping works for each use case.
The Mappings module is a powerful JSON-to-JSON transformation engine that helps you transform Guide JSON into and out of the shape you need for your business system. You can use Stedi’s visual mapper to build mappings for both inbound and outbound transactions.

Jan 12, 2024
EDI platform
You can now import your trading partner’s EDI guides directly from the Stedi Network when creating transaction settings. The Stedi Network has pre-built guides for hundreds of popular trading partners that you can use in your integration for free.
Stedi guides are a machine-readable version of the EDI requirements – sometimes called implementation guides – that your partner would typically provide as PDF, CSV, or Word documents. When you add a guide to a transaction setting, Stedi validates and translates (inbound files) or generates (outbound files) EDI according to the guide’s requirements.
Request guides: If you don’t see your partner’s guides in the Stedi Network, submit a request and we’ll build the guides you need for free in 1-2 business days.

Jan 3, 2024
EDI platform
You can now configure transaction.processed.v2 event bindings to trigger a Destination webhook based on the following new filters:
Connection: Inbound files from a specific connection. This option is useful when there are multiple connections within the same partnership. For example, you may set up a separate SFTP connection for test files and route them to a test endpoint.
Mode: The transaction contains a specific value in the ISA-15 element, which is used in X12 to distinguish between test and production files. This option is useful when you want to send test and production data to separate endpoints.
Destination webhooks allow you to automatically send data and events from Stedi to any external API. You can configure one or more event bindings that conditionally trigger each webhook. The new Connection and Mode filters are available under the Advanced menu.

Dec 18, 2023
EDI platform
You can now programmatically retrieve the generated EDI files that Stedi has delivered to your trading partner.
Stedi emits a file.delivered.v2 event every time a file is successfully delivered to a connection for an outbound transaction set. These events now include an output URL in an event.detail.artifacts object. You can use this URL to fetch the generated EDI file, including its envelope information.
Dec 14, 2023
EDI platform
You can now configure Remote FTP and FTPS connections in the Stedi app.
For each partnership configuration in your Stedi account, you can set up one or more connection protocols to exchange files. When connecting to your partner’s remote server, you can choose between the FTP, FTPS, and SFTP protocols.

Dec 6, 2023
EDI platform
You can now use Mappings to automatically transform file.processed.v2 events into a custom JSON shape. You can then attach the mapping to a Destination webhook to automatically forward transformed event data to your API.
For every successful file execution, Stedi emits a file.processed.v2 event that includes information about when Stedi processed the file, the associated partnership configuration, the file size, and more.
Visit the Events documentation for complete details.
Dec 1, 2023
EDI platform
Stedi Mappings is our powerful JSON-to-JSON transformation engine. We recently made the following major improvements to the visual mapping tool:
The visual mapper now shows warnings when the expected mapping output does not match the target JSON Schema. These warnings highlight issues such as invalid value types and missing properties to help you more easily create a complete, accurate mapping.
We added a quickstart workflow that makes it easier to create new mappings. You can choose a quickstart for reading EDI (mapping transactions from Stedi to a custom shape for your API), writing EDI (mapping JSON from your system to the shape required for Stedi’s Generate API), and ingesting Stedi events (for example, mapping `file.failed.v2` events to a custom shape).
To help you keep mappings up-to-date, we added clearer notifications when a connected Stedi guide has changed (for example, it has new segments or elements) and provided instructions for pulling those changes into your mapping.

Dec 1, 2023
EDI platform
You can now view detailed logs for each Destination webhook and filter them by a specific date range. The logs provide details about how the webhook is functioning, such as when each webhook is triggered and the response from the configured endpoint, which can help you troubleshoot issues.
Destination webhooks allow you to send transaction data and events from Stedi to any external API. To view the logs for a destination, click its name to go to its details page, and then navigate to the Logs tab.
Dec 1, 2023
EDI platform
You can now set a custom filename for autogenerated acknowledgments to comply with your trading partner’s requirements.
Stedi can automatically generate a 997 Functional Acknowledgment or a 999 Implementation Acknowledgment for each inbound transaction and deliver it to a specified connection.
To set a custom filename, navigate to the partnership, turn on the Acknowledgments functionality, and enter a JSONata expression into the Filename expression field. For example, the expression "EDI997_" & $millis()would produce filenames that start with EDI997 and then contain a timestamp, such as EDI997-5182341242.edi.
Nov 21, 2023
EDI platform
You can now specify a regex expression for Stedi to use when retrieving files from a Remote SFTP/FTPS connection. When polling the remote server, Stedi only processes files that match the filter pattern.
For example, your trading partner may place files for multiple different entities on the remote server, with different prefixes for each entity. In this case, you could write a regex expression that matches only files with a given prefix.
You can specify a Filter pattern for the remote poller in the connection’s Inbound settings.
Nov 21, 2023
EDI platform
You can now use Stedi mappings to automatically transform file.failed.v2 events into a custom shape before sending them to external APIs.
Stedi emits file.failed.v2 events when it cannot parse an inbound EDI file, or it cannot deliver an outbound EDI file to the configured connection. You may want to automatically send these events to an external platform like Slack or Jira, so your team can receive alerts and monitor issue resolution.
You can now create a Stedi mapping to transform the file.failed.v2 event JSON into the shape your external systems can receive and ingest. Then, you can attach the mapping to a Destination webhook to automatically forward the transformed event data to your API.
Nov 16, 2023
EDI platform
You can now attach files to any Stedi guide and choose whether the attachments are public or private (only available to members of your Stedi account).
Stedi guides are a machine-readable representation of the EDI specifications that your trading partners provide to you or that you provide to your trading partners. Attachments provide additional information about the guide.
For example, you may want to add private attachments that help your team debug issues in your EDI pipeline, such as the original PDF specifications or a changelog. For a public guide, you may want to attach an appendix with a supplementary code list or a diagram that helps your partners understand the messaging flow.
To add attachments to a guide in your account, navigate to its Overview page, scroll to the Attachments section, and click Attach file.
Nov 16, 2023
EDI platform
You can now use OAuth 2.0 with Destination webhooks.
Destination webhooks allow you to send transaction data and events from Stedi to any external API. To configure a destination webhook, you first create an auth configuration that defines how to authenticate with a set of URL endpoints.
The OAuth 2.0 configuration includes setting the Authorization endpoint and parameters, the HTTP method, a client ID, and a client secret. You can create a new OAuth 2.0 configuration from the Event Destinations page.
Nov 1, 2023
EDI platform
Your trading partner may send you TA1 Interchange Acknowledgments in response to outbound EDI files.
Stedi now automatically processes inbound TA1s and displays the data in the File executions and Transactions pages for inspection.
You can also set the acknowledgmentRequestedCode outbound EDI files to request interchange acknowledgments from your trading partner. Visit the Generate EDI docs for details.
TA1s indicate receipt of an interchange and identify any errors in the interchange's envelope (ISA and IEA) information.
Nov 1, 2023
EDI platform
Stedi accounts on the Enterprise plan can now set an automatic data removal time frame in Stedi.
Artifacts refer to the transaction and file execution payloads from files Stedi has processed. They contain the actual input/output transaction data in EDI, JSON, or another format. You may want Stedi to remove artifacts after a certain time frame - for example, to comply with your company's PII/PHI retention policies.
Once you set a retention period, Stedi deletes artifacts after the retention window has passed. This affects both existing and future data in your account.
For example, if you set a retention period of 30 days and process a file today, Stedi will delete the artifact after 30 total days have elapsed. Stedi will also delete any artifact created more than 30 days prior. For more details on how artifact retention works, please visit the docs.You can set an automatic data removal time frame from the Settings page.
Oct 30, 2023
EDI platform
You can now generate and send inbound test files to simulate receiving a file from your trading partner. This is useful for testing your downstream integration, since the inbound file will trigger configured destination webhooks.
To generate an inbound test file:
Go to the File executions page or navigate into a partnership and click Test inbound.
Select a partnership and an Inbound transaction setting.
Autogenerate the test file from a sample EDI file in the guide or paste your own test data into the editor.
Click Ingest file.
Stedi immediately processes the generated file and triggers any configured webhooks. You can review the results on the File Executions and Transactions pages.

Oct 24, 2023
EDI platform
Stedi provides fully-managed AS2 connections that take care of the intricacies of AS2 and scale automatically to meet your demand. We recently made the following improvements:
We added extensive conditional validation to reduce common configuration errors.
You can now view and filter provisioning logs for each AS2 connection. These logs detail each step to create or update the connection, such as provisioning the certificates, making it easier to diagnose errors. To view provisioning logs, go to the partnership associated with the connection, and then click the connection to view its details page.
When creating or updating an AS2 connection, Stedi now clearly indicates when there are previously uploaded encryption and signing certificates and provides the option to update them. Previously, adding or updating certificates was a separate workflow.
Oct 18, 2023
EDI platform
Stedi accounts on the Enterprise plan can now use fragments to split large transaction payloads from Stedi into smaller, more manageable chunks for downstream processing.
Large EDI files are often the result of transaction sets containing many repeated loops or segments. For example, a company may receive an 837 Health Care Claim file containing many insurance claims, or a retailer may receive an 846 Inventory Inquiry/Advice file containing millions of SKUs. To avoid overloading downstream systems, you can enable fragments on the repeated EDI segment.
Once enabled, Stedi splits the transaction payload into chunks based on that segment.For example, you might enable fragments on the LIN loop (list of inventory items) in an 846 Inventory Inquiry/Advice. For each processed 846, Stedi will emit fragment.processed.v2 events that each contain a chunk of LIN loop iterations.
You can create destination webhooks to automatically send fragment data to your downstream systems, or you can use the API to request the fragments for each processed transaction.
Oct 5, 2023
EDI platform
Stedi's guide builder now shows warnings when an ID element does not specify the set of allowed codes. You can see which fields are missing ID codes and specify the allowed values from the provided list or supply your custom codes.
Code warnings are available to help improve the quality of your guides, and you can ignore them without affecting Stedi's ability to use the guide for EDI processing. Warnings only appear for ID fields where the X12 specification includes the allowed code values. For example, they will not appear for State or Province codes.
Why element codes are important
ID element codes are a powerful component of the X12 EDI specification to provide additional information about data fields and reference well-known values. For example, you can use ID codes to specify the currency code of a monetary value, the meaning of a date value, or the reason for a shipment delay.
Many elements offer 1,000 or more possible codes, but most trading partners only expect to use just one or a few of these values. If a guide does not indicate which codes are accepted, trading partners often have to engage in costly follow-up with EDI departments or conduct multiple rounds of testing as they discover more code values in use.
The new warnings in Stedi's guide builder help ensure you and your trading partners work with the most accurate EDI specifications on the market.
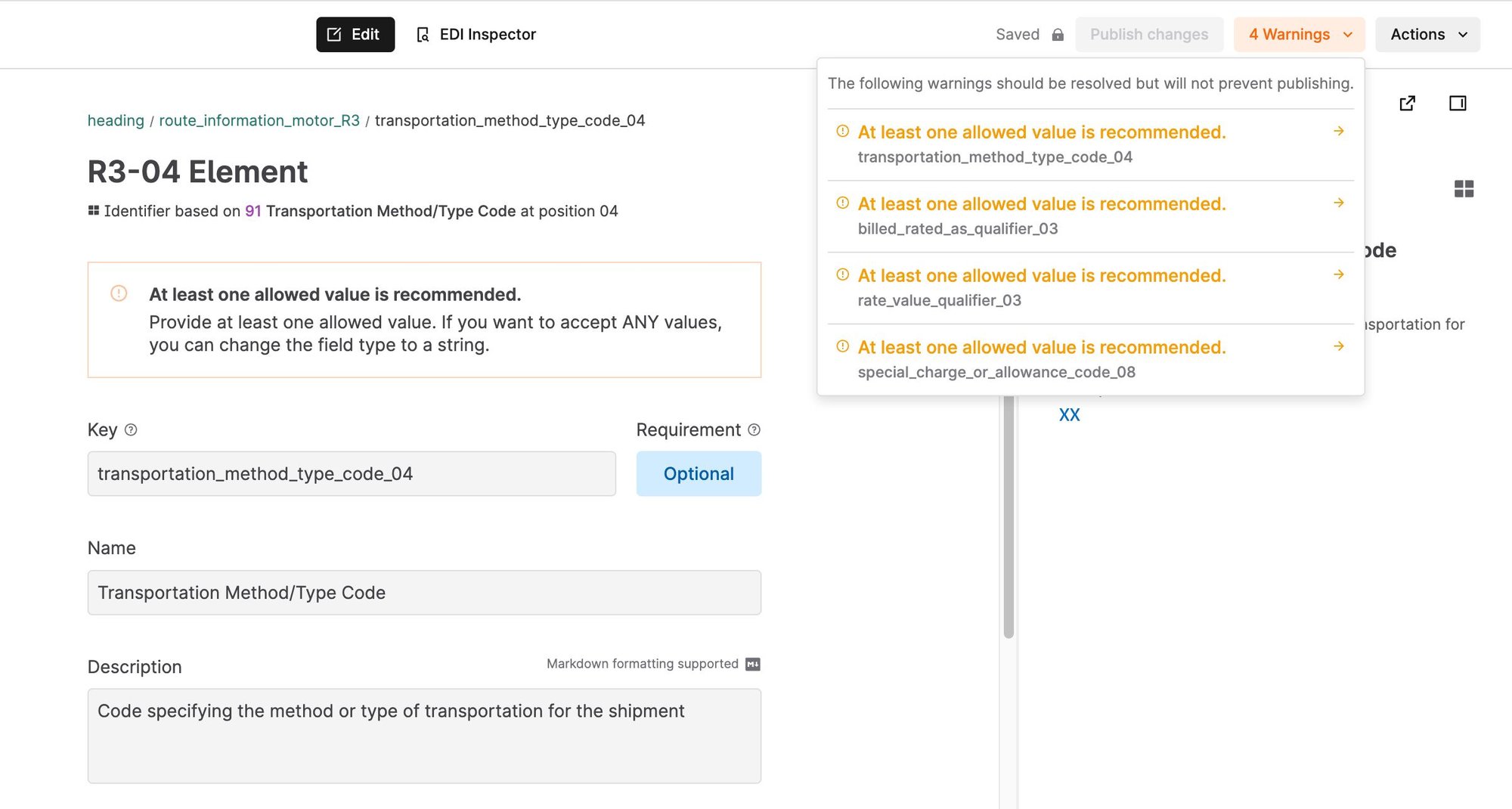
Pre-built guides: Instead of building guides from scratch, you can find hundreds of free guides for popular trading partners in the Stedi Network.
Oct 3, 2023
EDI platform
You can now add a mapping to destination webhooks to automatically transform transactions before delivering them to external APIs.Stedi parses EDI files into Guide JSON, which reflects the structure of an EDI transaction in a modern format. You can use a mapping to transform Guide JSON into the shape required by your internal systems and business applications. Mappings provide a visual interface for building JSON-to-JSON transformations and are available in the Cloud and Enterprise plans.
To add a mapping to a destination webhook:
Use the mappings editor to create a transformation for the
transaction.processed.v2event. Visit the mappings documentation for instructions.Select the mapping in the Mapping menu when creating a
transaction.processed.v2event binding. Visit the webhooks documentation for complete instructions.
Sep 28, 2023
EDI platform
You can now create partnerships faster by importing guides from the Stedi Network.
Partnerships contain transaction settings that define the EDI transaction sets you plan to exchange with that trading partner. For each transaction setting, you specify the EDI guide Stedi should use to validate data. The Stedi Network has pre-built guides for hundreds of popular trading partners that you can use in your integrations.
To import a partnership from the Stedi Network, go to the Trading partners page, click Create partnership, and choose Import from network. Visit the partnerships documentation for step-by-step instructions.
If you can't find your partner or guide in the network, you can submit a request, and we'll build it for you for free within 1-2 business days.

Sep 27, 2023
EDI platform
Stedi accounts on the Enterprise pricing plan can now use role-based access control (RBAC) to ensure only authorized users can access and modify account resources.
Admins can assign account members to one of four roles:
Admin: These users can access and modify all resources within a Stedi account. This includes adding and removing members, assigning member roles, adding billing information, switching between pricing plans, configuring Partnerships, generating EDI files, and configuring resources like Mappings and Functions.
Developer: These users can access and configure all resources, such as Partnerships, Mappings, and Functions.
Operator: These users can access and configure Partnerships, Guides, and Mappings. They can interact with developer resources like Functions, but cannot modify them. For example, they can invoke existing Stedi functions, but cannot change them or add new functions.
Read-only: These users can view account resources, but cannot modify them. For example, they can review processed transactions in Stedi's interface but cannot call the Generate EDI API or edit partnership details.
To change a member's role, go to Settings > Members in your account. Click the pencil icon for a member, choose a Role from the list, and click Update role.
Sep 24, 2023
EDI platform
You can now enable automatic 999 Implementation Acknowledgments for any Stedi partnership.
When you enable 999 acknowledgments for a partnership, Stedi automatically generates a 999 acknowledgment per functionality group of every valid inbound EDI file and delivers the 999s to your trading partner using the specified connection.
You will only use 999 acknowledgments in response to healthcare transactions. It's likely you should use 999s if you receive these transaction sets:
Each generated acknowledgment includes ISA and GS envelopes, complete with auto-incremented control numbers. Visit the partnerships documentation for more details.
Sep 14, 2023
EDI platform
The EDI Inspector in Stedi guides can now autogenerate an envelope for any sample EDI file.
If the EDI test file in the editor does not contain an envelope, the EDI Inspector displays a Generate envelope button that you can use to instantly create a generic envelope for the transaction set. You can then edit the envelope with information for you and your trading partner.Stedi guides are a machine-readable format for EDI specifications that Stedi uses to translate inbound EDI files and generate outbound EDI files according to your and your trading partners' requirements. You can use the EDI Inspector in each guide to validate EDI test files according to the guide's specifications. You can start from sample files attached to the guide or add your own test file into the editor.Check out the Stedi Network, which includes Stedi guides for hundreds of popular trading partners. You can import any guide into your Stedi account to use in your EDI integrations.

Sep 7, 2023
EDI platform
You can now set the maximum number of concurrent executions for any Stedi function to avoid overloading downstream services and ensure that the function can scale up as needed.
Concurrency refers to the number of in-flight requests your function is handling at the same time. With the new concurrency controls, you can set the maximum number of executions that a given function can execute simultaneously. Generally, you would set this to a number that your downstream system can comfortably support.
In addition to limiting the number of concurrent requests, concurrency controls help ensure that you always have available capacity for a given function within your Stedi account. All functions within a Stedi account share an overall concurrency limit that can be raised upon request. When you set a concurrency limit for a specific function, you reserve a part of the overall account "budget" for that function. This approach ensures that you can scale up to the reserved level, even if other functions are experiencing a high load.
To use this feature, go to the Functions UI, click the function you want to edit, and set the Max concurrent executions.
Sep 4, 2023
EDI platform
We are excited to announce that our EDI Inspector can now validate EDIFACT EDI files. All EDIFACT releases D96A and later are supported.
The EDI Inspector instantly recognizes any X12 or EDIFACT EDI file and validates its content against the corresponding EDI standard. You can view the transaction data on an easy-to-read UI, and identify and fix errors, such as incorrect codes and formats, missing or misplaced segments, and more.
EDIFACT integration preview: Soon, you'll be able to configure an EDIFACT integration on Stedi to exchange EDIFACT files with your partners. Contact us to get added to the preview launch.

Aug 31, 2023
Accounts
You can now configure your Remote FTP connections to use a static source IP address when exchanging EDI files with your trading partners.
Enabling a Static IP address ensures that your Remote FTP connections always use the same source IP address when communicating with the remote server. This may be required if one or more of your trading partners need to add your IP address to an allowlist to enable access.
You can enable a static IP address for your Remote FTP connections from the Core settings UI.
Aug 30, 2023
EDI platform
You can now generate and send test files to your trading partner from your browser.
To send a test EDI file from within a partnership, you can open the menu next to any outbound transaction setting and click Send EDI. You can also access this feature from the File Executions page.Stedi can autogenerate the input transaction payload (JSON) from any sample EDI file in the guide. You can modify this payload or paste your data into the editor. You can send the file from the browser or get the (HTTP) Generate API syntax for that payload. If you send the file, Stedi delivers the outbound test file to the connection, and you can review the results on the File Executions and Transactions pages.
Learn more about configuring new trading partners in our documentation.
Aug 29, 2023
EDI platform
You can now configure Destination webhooks to send data from Stedi to third-party services without writing any custom code.You can use destinations to send processed transaction data to your internal systems and business applications for further processing. You can also configure webhooks for other Stedi events, such as file processing failures. You can use this approach to trigger alerts in systems like Slack, PagerDuty, or Zendesk for further review.
Stedi can send webhooks to:
Custom applications using Basic, OAuth, or API Key authorization
Cloud functions, including AWS Lambda, Google Cloud Functions, and Azure Functions
iPaaS platforms, such as Zapier, Workato, or Tray.io
ERPs like NetSuite, SAP, or Oracle.
Aug 20, 2023
EDI platform
You can now use Stedi's fully-managed AS2 connections
to exchange EDI documents with your trading partners.The UI helps you quickly set up and test an AS2 connection for a trading partner. When you enable inbound messages, Stedi automatically processes EDI files received through the connection. When you generate EDI for a partnership
using the API, Stedi uses the AS2 connection assigned to the transaction to deliver the document to the trading partner. You can review the delivery status of all your sent EDI files on the file executions page.

Aug 17, 2023
EDI platform
You can now generate a Stedi guide from sample EDI files.

When you upload one or more EDI samples in the guide builder UI, it pre-populates a new guide based on the segments and elements present in the sample data. This allows you to fine-tune the guide into its final shape instead of starting from scratch. For example, you can add code values and optional elements that are not present in the sample files.
You can always use our pre-built guides from the Stedi Network, which includes guides for hundreds of popular trading partners. We add any requested guide within 1-2 business days.
Jul 30, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our network:
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Jul 26, 2023
EDI platform
You can now use the auto-configure option to create Stedi Core profiles and partnerships even faster by using existing EDI files.
When you upload a valid EDI file, Core extracts information from the interchange and functional group headers to generate two profiles - one for the sender and one for the receiver - that you can review before finalizing. Core can also optionally generate a partnership linking those two profiles.
is an event-driven EDI system that can validate, parse, and generate EDI for any trading partner. Core profiles contain information required to construct the EDI envelope that has information about the sender and receiver and the metadata of the interchange. Partnerships are a unique relationship between two profiles and describe all aspects of the EDI relationship, including which transaction sets the trading partners will exchange.
Jul 25, 2023
EDI platform
You can now enable automatic 997 Functional Acknowledgments for any partnership
within Stedi Core.When you enable 997 acknowledgments for a partnership, Core automatically generates a 997 Functional Acknowledgment for every valid EDI received and delivers the 997 to the partner using the specified connection.Core generates acknowledgments at the functional group level of the original inbound EDI, and each generated acknowledgment includes ISA and GS envelopes, complete with auto-incremented control numbers. Visit the Core documentation
for more details.
Jul 20, 2023
EDI platform
You can now review the generated events and function request and response payloads associated with every file execution and transaction within Stedi Core. You can use this information to quickly troubleshoot issues and understand how your data flows through Core.Core emits events
for every file, functional group, and transaction set it successfully processes. It also emits events when it delivers generated files and for processing failures.You can now review associated Core events on any file execution or individual transaction details page. You can expand each event to view its complete JSON payload and all the functions that event triggered. You can view the name of the associated event binding and whether the function execution was successful, along with the full request payload.
Jul 17, 2023
EDI platform
We released the following improvements to Stedi guides
and Stedi functions
:
The EDI Guide Catalog now has a dynamic search bar that allows you to filter by company name, industry transaction set, or guide name. You can import any guide into your Stedi account for free to use in your integrations.
You can now print all Stedi guides without having to make them public.
The Functions UI now allows you to adjust the log retention period for each function. You can choose a retention period from 1 day to 10 years.
Jul 14, 2023
EDI platform
You can now configure both Stedi-hosted and remote SFTP / FTPS connections from within Stedi Core. Connections tell Core where to retrieve and send files for each trading partner.
For SFTP connections, Stedi creates and hosts a fully-managed FTP server. You specify an inbound directory where your partners can add EDI files for Core to automatically process and an outbound directory where Core will deposit generated EDI files for your partners to retrieve. After creation, you can share the autogenerated SFTP user credentials with your trading partners to begin securely exchanging files.
For remote SFTP, you can choose how often Core polls for new files, and you can fetch files manually at any time for testing and troubleshooting. Core automatically deposits generated EDI files in the specified outbound directory.
Visit the connections documentation
for full details and instructions.
Jul 11, 2023
EDI platform
You can now retry failed outbound file executions in Stedi Core.
Previously, failed outbound file executions required an entirely new EDI generation request
. Now, you can retry outbound file executions individually or in bulk. You can review all the delivery attempts and previous attempts for a given EDI generation request in Core.Stedi Core
is an event-driven EDI system that does most of the heavy lifting for EDI integrations. Core can validate, parse, and generate EDI for any trading partner and provides complete visibility into your real-time transaction data.
Jul 5, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Jun 18, 2023
EDI platform
You can now define a scheduler to automatically invoke Stedi Functions
.Quickly set up a basic scheduler in the Functions UI that runs your function after a specific number of minutes, hours, or days. You can also define an advanced scheduler with custom expressions.
Use
rateexpressions to invoke a function at regular intervals, such as every fifteen minutes.Use
cronexpressions when you want to invoke a function periodically at a specific time, such as at 8:00 AM (UTC+0) every first day of the month.
Functions is a compute service that lets you run code without managing servers. You can use functions to respond to Stedi Core events, integrate Stedi with external systems, and define functionality to fulfill any EDI integration requirement.
Jun 14, 2023
EDI platform
The Stedi Core Generate API and SDK
have the following improvements:
The generate request now supports an optional filename parameter that you can use to specify the name of the generated EDI document.
The generate response now includes a globally unique fileExecutionID that you can use to track outbound EDI documents. Previously, the response only included an artifactId equivalent to the filename.
You can generate and send X12 EDI to any trading partner by providing JSON to the Core API or SDK. Core displays generated EDI files in the UI and delivers them to the destination specified in each partnership's settings.
Jun 7, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
Wiliams Sonoma
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Jun 2, 2023
EDI platform
You can create and manage Stedi Functions, such as those using external libraries, locally with the Stedi CLI and Functions SDK. The Functions UI now contains a Local Setup page with step-by-step instructions to help you get started. As part of this update, we removed the ability to edit code in the Functions UI.
The CLI now uses esbuild, which enables multi-file functions and allows you to use npm libraries in function code.
Editing files locally promotes the usage of source control.
Functions is a compute service that lets you run code without managing servers. You can use functions to respond to Stedi Core events, integrate Stedi with external systems, and define functionality to fulfill any EDI integration requirement.
May 18, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Import any guide from the catalog into your Stedi account for free and use it for your integration.
Submit a request for new guides from any trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.
Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
May 11, 2023
EDI platform
Stedi Core now supports translating EDI transaction sets up to 130mb in size, both using a custom guide and using the default X12 spec.
Previously, the limit was 90mb with a guide and 50mb with the default X12 spec.
Dimension Previous limit New limit File size 500 mb [^1] 500 mb (unchanged) Largest transaction set within a file without a guide 50 mb 130 mb with a guide 90 mb 130 mb
[^1] An EDI file can contain multiple interchanges, and each interchange can contain multiple transaction sets. The limit of what Core can process is generally dictated by the size of the largest EDI transaction set within the file, not by the file size itself.
May 2, 2023
EDI platform
Stedi Core now supports translating EDI files up to 500mb and individual transaction sets up to 90mb. This is more than 80x larger than the EDI Translate API's current limit.
Apr 24, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Apr 20, 2023
EDI platform
We added new HIPAA guides to our public catalog:
Post-adjudicated Claims Data Reporting: Professional (X298A1)
Post-adjudicated Claims Data Reporting: Institutional (X299A1)
Stedi’s X12 HIPAA guides are a free catalog of X12 HIPAA specifications that make it easier to understand, test, and translate healthcare EDI.
Browse interactive specifications for each transaction set, view sample transactions, and even validate EDI files in real time in your browser. Import any X12 HIPAA guide into your Stedi account and customize it to fit your integration use case. You can also use guides to programmatically validate and generate X12 EDI that conforms to the specifications.
Apr 13, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.Contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Apr 6, 2023
EDI platform
We are excited to announce the addition of guides for the following brands to our public catalog:
CN Rail
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request if you want us to add guides for any new trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.You can also contact us to add your guides to the catalog, so you can simplify onboarding for your partners.
Mar 30, 2023
EDI platform
Stedi guides are machine-readable EDI specifications that you can share as interactive web pages with built-in X12 EDI validation. Stedi mappings let you transform JSON from one shape to another. You can base the source or target schema of a mapping on a guide, which lets you automatically pull changes from the connected guide into the mapping.
We recently released the following Guides and Mappings improvements and fixes:
Improvements
You now receive a warning when you try to delete a guide that is connected to one or more mappings. The warning lists all of the connected mappings.
The guide builder now includes tooltips when you hover over the colored icons next to each node in the sidebar. The tooltips tell you the segment or element type and whether or not it’s required.
The mappings UI now pre-selects all target keys when you create a mapping externally from the API or guide builder. Previously, Mappings only pre-selected target keys when you created a mapping from within the Mappings UI.
Fixes
When you enter Allowed Values for elements, the guide builder displays a shortened versioned of long JSON keys so they don't overlap with the description.
The guide builder now allows spaces in values. This update is important for values like organization names, which require spaces for readability.
Mar 28, 2023
EDI platform
The EDI Guide Catalog is an open directory of our most-requested public Stedi guides, interactive EDI specifications that let you instantly validate X12 EDI documents.
We are excited to announce the addition of guides for the following brands to our public catalog:
Stedi guides contain validated sample files to help trading partners learn valid usage patterns faster. You can also use Stedi guides to automatically validate, parse, and generate EDI documents according to partner-specific requirements.
Submit a request for new guides for any trading partner, and we'll add them to the catalog for free. Building new guides typically only takes a few business days.You can also contact us to add your existing guides to the catalog.
Mar 27, 2023
EDI platform
While building a Stedi mapping
, you often need to omit a specific field based on the data in the incoming source document. For example, you may need to omit a delivery address object completely if the purchase order has not been confirmed yet. Now, you can use the $omitField constant
to omit both primitive fields and entire objects.Previously, Mappings UI only allowed using the $omitField for primitive fields (fields that map to strings, numbers, and booleans).You can now use $omitField to exclude an entire object or an array based on a condition. Mappings now recognizes $omitField within list context expressions
. In addition, every object field has a new optional object context input
with built-in support for $omitField.

Mar 23, 2023
EDI platform
EDI Translate uses Stedi guides to read, validate, and generate EDI according to partner-specific requirements. When you call EDI Translate APIs, you must provide your Stedi API key for authorization and either the EDI document (reading) or JSON document (writing EDI).
The guide builder now auto-generates sample EDI Translate API calls for reading and writing EDI. Click Actions > Get Translate API snippet to copy sample calls for several languages, including cURL, HTTP, and Python.
The sample API calls include valid test EDI or JSON data based on the guide's specifications. The guide builder auto-generates generic test data, but you can also get test data from an attached sample EDI file.
Mar 21, 2023
EDI platform
The Stedi bootstrap repository lets you quickly deploy a reference implementation that sends and receives EDI documents, connecting Stedi products in an end-to-end flow.
The bootstrap implementation now supports polling remote FTP / SFTP servers for new files. When the poller finds files, it copies them to a Stedi bucket and optionally deletes those files from the remote server. You can configure the bootstrap module to process these files automatically. Visit the bootstrap external poller README for more details.
Book time with our technical team for help deploying the bootstrap repository to your Stedi account and customizing it for your use case.
Mar 16, 2023
EDI platform
Building a Stedi mapping requires defining a source and target JSON schema. You can generate these schemas automatically by connecting the mapping to an existing Stedi guide.
Now, the Mappings UI shows you which mapping source or target schemas are connected to Stedi guides and links directly to the connected guide. This new view helps you understand how many mappings are linked to Stedi guides and which mappings are affected by specific guide changes.

Mar 15, 2023
EDI platform
Stedi Mappings let you transform JSON documents from one structure to another. By default, the Mappings API does not apply any payload validation on the /map endpoint.Now, you can enable Strict validation mode to validate the input and the output payload of the mapping operation. Validation helps you ensure that the mapping results are accurate and catch deviations from expected results early.To apply strict validation
, set the validation_mode query parameter to strict. Mappings uses the source schema
to validate the input document and the target schema
to validate the outgoing document.If validation of the input or output payload fails, the response is a 400 error with the validation_failed code and validation_errors object.
HTTP/1.1 400 Content-Type: application/json { "code": "validation_failed", "message": "The input of the mapping does not conform to the specified source JSON Schema, and the output of the mapping does not conform to the specified target JSON Schema.", "validation_errors": { "source": { "mapping_input": { "quantity": 15, "unit_price": 2.50 }, "errors": [ { "code": "required", "message": "must have required property 'unit_description'", "json_pointer": "/", "json_schema_pointer": "#/required" } ] }, "target": { "mapping_output": { "total": 37.50 }, "errors": [ { "code": "type", "message": "must be integer", "json_pointer": "/total", "json_schema_pointer": "#/properties/total/type" } ] } } }
Mar 9, 2023
EDI platform
You can include multiple EDI sample files in Stedi guides to help new trading partners understand valid usage patterns faster and reduce onboarding time.
Now, you can add a description to each sample that gives trading partners even more context about the intended use cases. The description appears at the top of the guide’s EDI Inspector.
This feature is available both for Public Guides and for Stedi guides published privately. View descriptions for samples in the YRC Freight X12 Motor Carrier Bill of Lading.



Mar 6, 2023
EDI platform
Stedi mappings let you transform JSON data from one shape to another, most importantly between your internal schema and EDI-like JSON required for EDI Translate.We launched the following improvements to the Mapping builder UI:
When you connect a Stedi guide to the mapping’s source or target schema, the Guide tab links directly to the connected guide.
The Schema and Example tabs are now read-only when a guide is connected. This prevents you and collaborators from manually editing the schema out of sync with the connected guide.
You can use the View menu to show and hide the source and output columns as needed.

Mar 3, 2023
EDI platform
The industry identifier for an EDI transaction set is specified in characters 7-12 of the GS-08 element of the functional group header.
You can now change the industry identifier when building a custom Stedi guide for an X12 HIPAA transaction set. You can build a custom guide by importing an X12 HIPAA public guide into your account. EDI Translate uses the industry identifier you choose when generating EDI documents according to your guide's specifications.

Mar 1, 2023
EDI platform
Delimiters separate the segments and elements in an EDI file. When you create a Stedi guide, you can choose the delimiters that the EDI Translate API should use when writing EDI.
Now, you can choose underscore as the delimiter option in Stedi guides.
Visit our product documentation for more information about delimiters in Stedi guides.
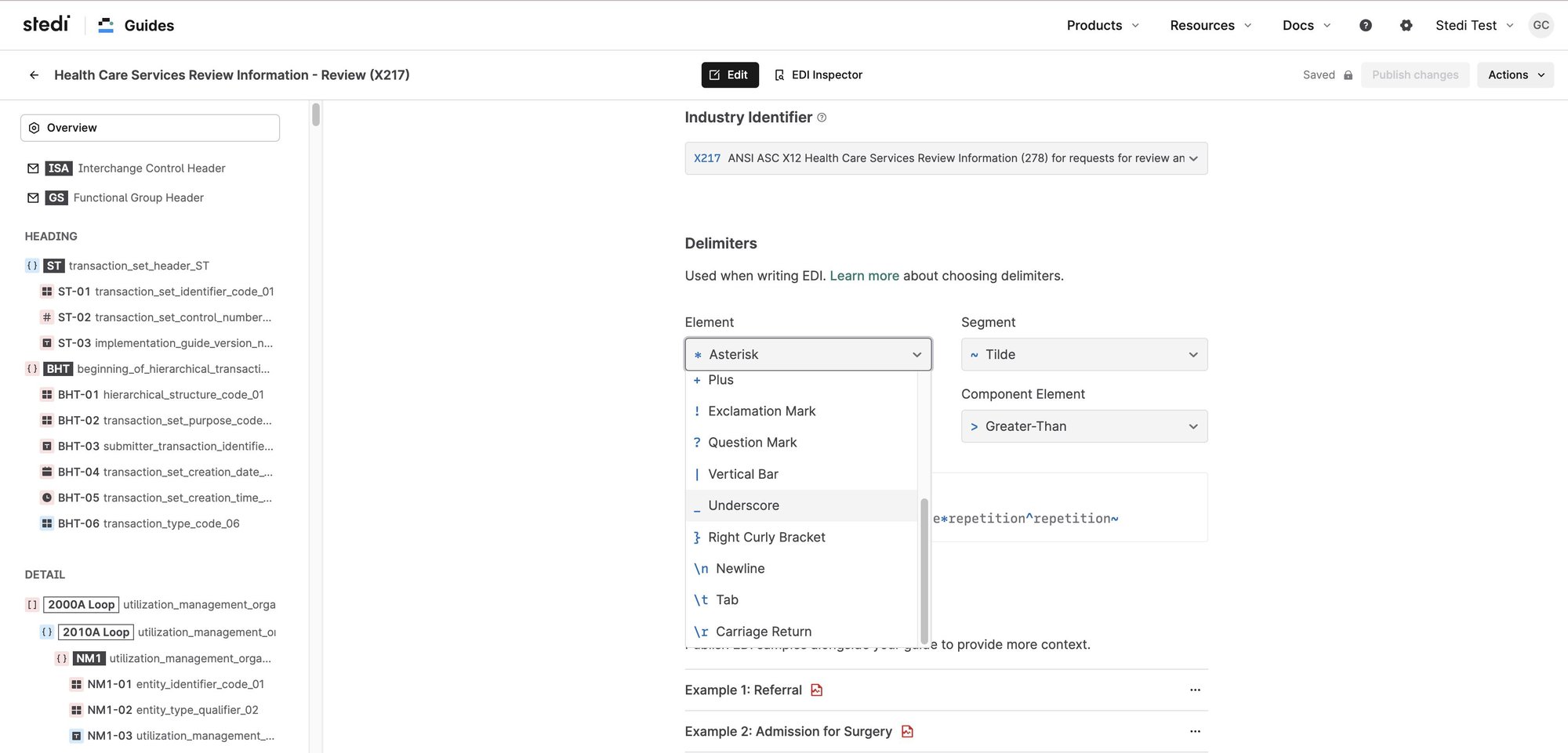
Feb 27, 2023
EDI platform
Stedi guides let you view and share EDI specifications as interactive web pages with built-in X12 EDI validation. You can also download Stedi guides as high-quality PDFs.
EDI samples attached to the guide are now included in the downloaded PDF.
The guide builder automatically validates new sample files against the guide specifications, so you can be sure that the sample matches the specification before sharing the PDF with your trading partners.

Feb 22, 2023
EDI platform
We are excited to announce the availability of Stedi’s X12 HIPAA guides, a free catalog of X12 HIPAA specifications that make it easier to understand, test, and translate healthcare EDI.
Browse interactive specifications for each transaction set, view sample transactions, and even validate EDI files in real time in your browser. Import any X12 HIPAA guide directly into your Stedi account and customize it to fit your integration use case. You can use Stedi's EDI Translate APIs to programmatically validate against any X12 HIPAA guides as well as parse and generate X12 EDI that conforms to the specifications.
Feb 16, 2023
EDI platform
Stedi guides and EDI Translate convert data between EDI and EDI-like JSON. Stedi mappings transform data between EDI-like JSON and a custom JSON shape that reflects your internal data model.
Each mapping has a source schema and a target schema, which you can define based on a Stedi guide or a sample JSON file.
Now, the mappings UI automatically detects changes in connected Stedi guides and lets you pull those changes into the schema. When you change the schema, the mappings UI alerts you when the updates affect existing expressions in the mapping.
Feb 14, 2023
EDI platform
Stedi EDI Inspector instantly recognizes data from any X12 EDI file and validates it against the standard to catch errors such as incorrect codes and formats, missing or misplaced segments, and more. Each Stedi Guide has a built-in EDI Inspector that validates files against partner-specific EDI specifications. Now, you can download validated EDI files.
Try the EDI Inspector on Walmart's 204 Motor Carrier Load Tender. Visit the EDI Guide Catalog for public guides from many trading partners, including Amazon, FedEx, Walmart, Trader Joe's, and more.
Feb 6, 2023
EDI platform
The first step toward building an EDI integration with Stedi is to create a Stedi guide from your partner's PDF implementation guide. Now, you can skip this step and directly import any guide from our EDI Guide Catalog into your Stedi account to integrate faster.
The EDI Guide Catalog is an open directory of our most-requested guides, and we continue adding more. You can view these guides as interactive EDI specifications and validate test files right in your browser. You can also request new guides, and we'll add them to the catalog.
Feb 2, 2023
EDI platform
A Stedi mapping lets you transform data into any JSON shape you want. Now, you can create a mapping directly from a Stedi guide for EDI reading or writing use cases.
Mappings are useful when you want to transform data to or from EDI-like JSON. For example, you may need to transform data from the guide JSON format that EDI Translate understands into a custom shape for internal systems. EDI Translate uses guides to quickly and accurately convert data between EDI and JSON. The JSON shape for both input and output closely matches the shape of the incoming or outgoing EDI.
Jan 30, 2023
EDI platform
We're constantly simplifying the guide builder experience. Instead of adding allowed values one-by-one for code (Identifier) elements, you can now provide a comma separated list of all the values you want to allow.
For the Currency Code, you can now select from a dropdown of standard ISO codes. This minimizes the chances of errors in the specification from entering an invalid code.
Jan 27, 2023
EDI platform
You may want to allow multiple variants of a segment or loop in your EDI specifications. For example, you could specify that partners include two N1 Name loops in each 850 purchase order: one for the ship to contact and another for the bill to party.
The guide builder UI now lets you select a discriminant element that has unique values for each variant. The discriminant tells the guide’s EDI Inspector and the EDI Translate API when one variant should be used over the other for validating, generating, or parsing EDI documents.
In the 850 purchase order example, you’d add the Entity Identifier Code as the discriminant for N1 Name loops. For the bill to variant, you’d use the BT qualifier, and for the ship to variant, you’d use the ST qualifier.
Jan 26, 2023
EDI platform
Formatting a malformed EDI file can be painful, especially if you are new to EDI or when you are troubleshooting a problem. This is why we originally introduced the 'Format' option on the EDI Inspector to make EDI content easier to navigate.
We noticed that EDI samples enclosed in PDF implementation guides almost always have incorrect whitespace padding within the ISA header. A customer needs to manually correct these to get to a valid EDI even if the rest of the EDI document is valid. Starting today, the format action detects the whitespace issues within the ISA header, and recommends one-click fixes to quickly get to a valid EDI. Try it out on a sample guide today.
Jan 25, 2023
Accounts
We are excited to announce that Stedi has successfully passed an external audit and our products have been certified as HIPAA eligible. This certification means that our products have undergone rigorous testing and have been deemed compliant with HIPAA regulations.
We understand that HIPAA eligibility is important for our customers in the healthcare industry as it ensures their sensitive patient data and protected health information (PHI) will be safe and kept confidential when using Stedi products. This is critical when you are exchanging health information such as claims, eligibility, and enrollment information with your partners.
This certification is just one of the many ways in which Stedi is fortifying its platform to handle customer data safely and securely. Visit our trust page for more information on our security and compliance policies and documents, or contact us with any compliance questions related to your business case.
Jan 25, 2023
Accounts
We are excited to announce that Stedi has received SOC 2 Type II compliance certification. This certification demonstrates our commitment to maintaining the highest standards of security, availability, and confidentiality for our customers’ data.
SOC 2 Type II certification is a rigorous and comprehensive evaluation process that assesses a company’s internal controls and security practices to protect customers’ sensitive information. We will continue to undergo independent audits at regular intervals to verify our compliance.
This certification is just one of the many ways in which Stedi is fortifying its platform to handle customer data safely and securely. Visit our trust page for more information on our security and compliance policies, or contact us with any compliance questions related to your business case.
Jan 23, 2023
EDI platform
Stedi creates building blocks for custom, end-to-end EDI integrations. Now, our bootstrap repository lets you quickly configure and run a sample implementation that reads and writes EDI documents from your Stedi account.
The bootstrap implementation uses the following steps to handle inbound EDI:
You add EDI documents to a Stedi Bucket.
New EDI documents automatically invoke a Stedi Function that processes this data payload.
The function calls the EDI Translate API to transform the EDI data into JSON. The transformation requires a Stedi Guide to map EDI fields to JSON fields.
The function sends the JSON document to a webhook.
The bootstrap implementation has a similar workflow for generating outbound EDI. Your EDI flows may differ from these simple examples, but the bootstrap is an excellent starting point for your first integration. We encourage you to Contact us as you get started with Stedi, so our team can help you customize the bootstrap workflow for your use case.
Jan 20, 2023
EDI platform
EDI is really hard. We’re here to help!
Introducing the Stedi EDI Forum: A public resource for sharing EDI questions, complaints, and ideas with Stedi experts and the EDI community. You can also use it to provide feedback about Stedi products.
Everyone can view the forum for free, and you can create a free Stedi account to contribute.
Jan 19, 2023
EDI platform
EDI sample files convey pages worth of specifications in a single snapshot. They help new trading partners understand valid usage patterns faster and reduce debugging time.
You can now add up to five EDI samples in each Stedi guide to represent supported variants. The guide builder automatically validates new sample files against the guide specifications, so you can fix errors before providing them to your trading partners.
After you add samples, your trading partners can view and edit them directly in their web browsers.

Jan 12, 2023
EDI platform
We are excited to announce the EDI Guide Catalog, an open directory of public Stedi Guides for a wide range of trading partners and industries. Stedi Guides provide EDI specifications as interactive web pages and also let you validate X12 EDI documents in your browser.
The catalog contains guides for our customers’ most-requested trading partners, which include companies like Walmart and FedEx. We build and maintain these guides to support customer integrations and provide them as a reference to the larger EDI community.
Access to the catalog is free. We will continue to add to this list, although you can also build custom guides to integrate with any trading partner not listed here. Contact us for a demo or with any questions.

Dec 16, 2022
EDI platform
You can now use our reference implementation for inventory feed processor and SFTP poller to jumpstart your own implementation rather than starting from scratch. These examples use Stedi Functions SFTP (backed by Buckets), and Stash. You can also use the ideas in these reference architectures to develop a unique architecture of your own.
Also, the Stedi bootstrap repository contains a reference implementation for both an inbound EDI workflow and an outbound EDI workflow.
Dec 16, 2022
EDI platform
You can now easily switch between Public Guide specifications and the built in EDI Inspector using the new navigation bar. The navigation bar also has options to share the guide and share a link to your EDI inspector view, along with the EDI file and the validation results.
Try it on a sample Public Guide, or build your own guide today.

Dec 16, 2022
EDI platform
You no longer have to hand edit relational conditions for a segment when building a Stedi guide. You can use a form-based interface to add or update conditions and the X12 condition code is automatically generated for you.

Dec 14, 2022
EDI platform
We are pleased to announce a 90% price drop for Buckets LIST requests, taking the price down from $0.50 to $0.05 per 1000 requests. With this reduction, a LIST request will now cost you the same as a GET or a SELECT request (see buckets pricing). The new pricing is effective as of Dec 14, 2022
If you use Stedi’s serverless SFTP, this results in direct savings when trading partners poll your SFTP directory to check for new files, as SFTP issues LIST requests to the underlying Stedi bucket on your behalf.
Dec 9, 2022
EDI platform
The X12 EDI Standard contains several figures that require special formatting. You can now view the guidance and structure of these figures in the context of elements, segments, and transaction sets where applicable on Stedi’s EDI Reference.
Elements: C001 Composite Unit of Measure, 347 Hash Total, 758 Hazardous Materials Code
Segments: CUR Currency, CTP Pricing Information, LE Loop Trailer, LS Loop Header
Transaction sets: 141 Product Service Claim Response, 837 Health Care Claim.
Dec 8, 2022
EDI platform
EDI Inspector on Stedi Guides allows you and your trading partners to test EDI files against the guide. EDI Inspector now performs this validation without your EDI content ever leaving your browser. Any pasted EDI content in the EDI Inspector stays on your machine and is never sent over the wire. Local validation also means you get an extremely responsive interface that gives you real-time feedback as you troubleshoot and update your EDI content.
This is now the default behavior of EDI Inspector on all guide pages (including Public Guides), and the EDI Inspector on guide builder UI. Try out EDI Inspector on a sample guide here.
Dec 8, 2022
EDI platform
You can now access logs and metrics for Stedi Functions directly in the Functions web UI. Logs are useful for troubleshooting test and production workloads, and the metrics provide an insight into your functions’ performance over time.
Logs and metrics for Functions are available in public preview, which means we’re actively improving the feature. Functions is generally available - you can read more about how Functions can help with your EDI integration in this blog.
Dec 7, 2022
EDI platform
We’re announcing a 100% price cut for API request pricing for Stash, a key-value store designed for any EDI workflow or B2B integration. You are no longer charged any fixed amount for the number of Stash API requests. This change is currently in effect (since Nov 2022 billing cycle).
You are only charged for the read and write units, and for the storage of data. The pricing for these dimensions remains unchanged from before (see pricing).
Dec 1, 2022
EDI platform
There is nothing like having an organized view when you’re analyzing data. This is especially true for testing and troubleshooting EDI files. With the EDI Inspector on Stedi guides, you can now format your EDI content with the click of a button to make it more legible. For example, you can use this option on a single-line EDI file to display each segment in a separate line.
The format button is available with the EDI Inspector on all Stedi guides, including Public Guides pages.
Nov 28, 2022
EDI platform
You can now add optional usage notes to any segment, loop, or element within your Stedi guide. Usage notes can also be added to individual codes for an identifier (ID) type element to convey additional context. Usage notes are rendered as part of your Public guide, and provide your trading partners guidance specific to your business beyond the standard X12 descriptions.
For example, your logistics company has a custom numbering scheme for stop sequence for Motor Carrier Load Tenders (204) and Freight Invoices (859), or your Healthcare Claim (837) specification requires a partner to provide geographic location as city + 2-character state code + 9-digit zip code. This information can now be conveyed via usage notes for your trading partners to review as they onboard.
Usage notes are also rendered when viewing the guide privately by any member of your Stedi account. You can add usage notes to any Stedi guide using the guide builder UI.

Nov 28, 2022
EDI platform
You can now create a Stedi guide directly from the EDI Inspector page. Besides validating an EDI sample, EDI Inspector will now present an option to create a Stedi guide for the specific transaction set of the EDI sample. Upon choosing this option, you will be taken to the guide builder UI with the X12 release version and transaction set pre-selected for you. You can continue after this jumpstart and complete the guide based on specifications from your trading partner.
For more details on creating a Stedi guide, check out our user guide.

Nov 18, 2022
EDI platform
Every EDI message contains an interchange envelope, with one or more transaction sets nested inside the interchange. The transaction set contains the actual content of the message.
Previously, customers using EDI Translate to generate EDI from a JSON payload could only generate a single transaction set inside of an interchange. Now, customers who want to “batch” multiple transaction sets inside a single interchange can do so using the same API by passing an array of transaction sets in the JSON payload.
There is no additional charge for generating EDI with multiple transaction sets, you only pay for the request and the data processed (see pricing).
Nov 18, 2022
EDI platform
Customers can now view all historical transactions in the billing dashboard by navigating to the transactions section. View and download all historical transactions such as invoices, credit notes, and payments.
Nov 15, 2022
EDI platform
Starting today, you can modify a Stedi guide with confidence knowing you can always revert to the last published version. This option is available from the “Actions” menu on the guide builder UI. You no longer have to keep track of your changes if you ever need to discard them to get back to a known published state of the guide.
Nov 15, 2022
EDI platform
Public Guides comes with a built-in EDI inspector allowing customers to validate and troubleshoot EDI files against specifications right in the browser.
Starting today, in addition to highlighting the validation error, EDI Inspector also provides an option to update the EDI file with a suggested fix. This allows customers to quickly resolve issues, without having to refer back to the specifications. Try it out on a sample public guide, or build your own guide today.
Nov 15, 2022
EDI platform
Public Guides is a radically new and improved way for businesses to share EDI specifications and speed up the trading partner onboarding process. It features a built-in EDI inspector for validation and troubleshooting of EDI files against specifications right on the browser.
Now, Public Guides lets you share a link to your EDI inspector view, along with the EDI file and the validation results. By clicking the link, a recipient can load up the same file in the public guide’s EDI Inspector view, and they will see the same validation results (including any errors). This helps overcome communication gaps in describing validation issues over email, and the need to send EDI files back and forth. Try it out on a sample public guide, or build your own guide today.
Nov 14, 2022
EDI platform
eading and writing EDI is at the core of any EDI system. Stedi makes this easy with Guides, a way to define machine readable EDI specifications, and EDI Translate, an API to generate and parse EDI conforming to those specifications. Additionally, customers can use Mappings to transform data from the guide JSON Schema to their internal schema for inbound EDI (or vice versa for outbound EDI).
Previously, the guide builder UI exposed a single, generic JSON Schema for the guide. Customers using this guide JSON Schema for mapping had to make minor modifications depending on whether they are using the schema for EDI reading or EDI writing. Starting today, customers can access schemas specifically tailored for reading or writing EDI (in addition to the generic schema). The schemas can be used directly with Mappings without any modifications, or within your own mapping solution.
Nov 10, 2022
EDI platform
Public Guides is a radically new and improved way to share EDI specifications and speed up trading partner onboarding. A public guide is a live, interactive web page that is accessible by anyone with a link. Links can be shared directly with trading partners or included in an EDI portal – they provide the same information as a traditional PDF guide, but allow users to instantly validate and troubleshoot EDI files right in the browser using the EDI Inspector.
Previously, EDI Inspector required users to sign in to validate EDI files. We now removed this authentication step to make it easier for your trading partners to onboard with you. Trading partners can still optionally sign up for a Stedi account to access valuable EDI resources, including full-fledged EDI Reference and public EDI Inspector. Build your public guide today.
Nov 8, 2022
EDI platform
Stash is a key-value store designed for any B2B integration or EDI workflow. You can use Stash to track transactions processed, increment control numbers, reference lookup tables, and more - all using a simple API.
As of November 2022, Stash API requests are charged at $0.055 per 1,000 requests, a 75% reduction from the previous price of $0.22 per 1,000 requests. This applies to all customers with usage above the free tier (1,000 requests per month). The pricing for read and write volumes, and data storage remains unchanged. See pricing.
Nov 3, 2022
EDI platform
Public Guides is a radically new and improved way for businesses to share EDI specifications and speed up the trading partner onboarding process.
A public guide is a live, interactive web page that is accessible by anyone with a link. Links can be shared directly with trading partners or included in an EDI portal – they provide the same information as a traditional PDF guide, but allow users to instantly validate and troubleshoot EDI files right in the browser. An intuitive UI and helpful error messages lead them to quickly build EDI files that conform to the guide’s specifications, reducing the testing process from weeks to hours – and eliminating dozens of back-and-forth emails.
Oct 28, 2022
EDI platform
You can now view and customize ISA (Interchange Control Header) and GS (Functional Group Header) segments of the X12 envelope within a Stedi guide using the guide builder interface. These customizations are reflected in the interactive documentation of a Stedi guide, and are not used for validation by the EDI Translate API.

Oct 26, 2022
EDI platform
EDI Translate is a new API for creating and validating EDI files that conform to precise trading partner specifications. EDI Translate accepts user-defined JSON payloads and translates them into valid EDI files, and vice versa.
EDI Translate works in conjunction with recently-launched Stedi Guides, which enables users to quickly and accurately define EDI specifications using a no-code visual interface. Once a guide has been defined, users can use the EDI Translate API to create outbound EDI files that conform to the guide. Users can also use EDI Translate API to validate that inbound EDI files meet the defined specification, as well as parse these EDI files into JSON for further processing.
EDI Translate is now generally available. Read more.
Oct 19, 2022
EDI platform
Stedi Guides is our new product that enables you to quickly and accurately create EDI specifications using a visual interface. These specifications can be used to programmatically parse and generate EDI documents via the EDI Translate API using a modern JSON Schema format, or to validate EDI manually in a web browser against interactive documentation. There is built-in support for all X12 transaction sets and releases, and the ability to customize specifications beyond the strict X12 interpretation.
Stedi Guides is now generally available. Read more.

Sep 12, 2022
Accounts
You can now use Stedi's serverless SFTP infrastructure to securely exchange files with trading partners via FTPS as well. Provision users in seconds via the Stedi dashboard or the API. The same credentials can be used for both SFTP and FTPS. Read more.
Aug 29, 2022
EDI platform
If you receive data which contains a certain string but has a range of available prefixes or suffixes, and you need to map it to a reduced set of target values, you can use Lookup Tables with wildcards to match multiple possible input options at once. Simply replace the interchangeable part of the key with * symbol. Follow a step-by-step guide here.
Aug 28, 2022
EDI platform
Stedi Converter API is now deprecated. You can achieve conversions between any two data formats using Stedi Functions and a library of your choice. This tutorial explains how to deploy functions with the CLI. Please contact us if you need help with your implementation.
Jul 11, 2022
EDI platform
Stedi SFTP is a serverless SFTP endpoint for exchanging files at any volume. Provision users via SFTP UI or via the API and begin transferring files in seconds.Stedi SFTP is fully integrated with Stedi Buckets - a simple, reliable data store. When you upload files programmatically via the Buckets SDK
, those files are available to your trading partner via their SFTP credentials. And each time your trading partner uploads files via SFTP, those files are available via the Buckets SDK, too.
With a usage-based pricing model and no servers to manage, developers can easily offer SFTP connectivity to their trading partners as part of a new or existing B2B workflow without incurring fixed costs or operational overhead.
Create a serverless SFTP user in 20 seconds or less:

Jun 1, 2022
EDI platform
Edit JSON Schema in the Mappings UI
You can now upload and edit JSON Schema directly in the Mappings UI. Any changes in field descriptions will be automatically reflected on the mapping canvas.

In cases when JSON Schema conflicts with a JSON example after an update, you will be able to decide whether you'd like to re-generate the JSON Schema based on your new example or update your JSON Schema yourself.

Navigate source and target more easily with tree view
The source/target documents are now displayed in tree view to make it easier to navigate through large files. You can also use the search bar to quickly find the field you're looking for.

Improved autocomplete suggestions for values
Now, when you work with complex JSONata expressions that require filtering objects in arrays, you will see autocomplete suggestions for values in the predicate expressions.

Higher limits
We have increased the size limits for Mappings APIs to the following values:
Mapping source JSON Schema - 300 KiB
Mapping target JSON Schema - 300 KiB
Mapping JSONata expression - 300 KiB
Lookup tables combined size - 300 KiB
May 29, 2022
EDI platform
Now, when you work with complex JSONata expressions that require filtering objects in arrays, you will see autocomplete suggestions for keys in the predicate expressions.

Apr 24, 2022
EDI platform
2 weeks ago we launched the JSONata playground, which allows users to experiment and learn the JSONata language used by Stedi Mappings with a free online tool. Now, with the JSONata embed functionality, we have replaced all of our JSONata examples in our documentation to use the same editor that is in the playground.
See this in action with our JSONata cheatsheet.

Mar 24, 2022
EDI platform
Mappings: List indexes bank
If the list entries of your target document are expected to include a list index number, you can now access it by binding a positional variable to the List Context. You can read more about the positional variable binding in the JSONata docs. To learn more about list indexes and see examples, read our documentation here.

Mappings: JSON Schema preview in Mappings UI
When you define a Source and Target JSON in the Mappings UI, these shapes are automatically converted to JSON Schema on the backend. Now, you can navigate to this JSON Schema directly in the Mappings UI. By using JSON Schema, you get a more precise description of the structure and validation constraints of your JSON documents.

Mar 10, 2022
EDI platform
EDI Core, Mappings, and Converter are now HIPAA eligible. Developers can now use Stedi’s APIs to build business integrations and process transactions that contain Protected Health Information (PHI).
To start building HIPAA eligible systems using Stedi you will need to agree to a HIPAA Business Associate Addendum (BAA) with Stedi. To establish a BAA with Stedi, or if you have any other questions, please contact us.
Mar 4, 2022
EDI platform
Since launch, Mappings served traffic from a single geographic region. Now, Mappings serves traffic from multiple regions. This will increase the reliability of the service in the case of a regional outage, and decrease latency for requests made geographically closer.
Feb 25, 2022
EDI platform
Requests to Stedi APIs are authenticated using a secret token called an API key. Each API key belongs to a single account and each account can have multiple API keys. API keys can be created inside of the Stedi UI by navigating to the API keys tab.
With the launch of the API for creating, listing, and deleting API keys, you can now manage this process programmatically. To learn more, you can read our documentation.
Feb 22, 2022
EDI platform
Prettier is an opinionated code formatter. It enforces a consistent style by parsing your code and re-printing it with its own rules that take the maximum line length into account, wrapping code when necessary.
Since developers use JSONata in the Mappings product, Stedi has contributed to Prettier by adding the prettier-plugin-jsonata, which uses the JSONata parser available as part of the jsonata package.
Here is what JSONata looks like in the Mappings expression editor before formatting:

…and after formatting:

Feb 11, 2022
EDI platform
Converter is an API that allows developers to convert various formats like CSV and XML to JSON, providing a hassle-free way to manage these conversions. Converter has a transparent, pay-per-use pricing model with a generous free tier. There are no minimum fees, monthly commitments, or upfront costs to use this product.
In the example below, the Converter API uses the headers in the CSV as keys in the JSON. The result is a list with an object for each row, where the object has a field for each column. So, if you have a CSV like this…
type,invoiceNumber,poNumber,amt invoice,INV20023,30278099,100.50 invoice,INV20024,30288899,50.99
…the resulting JSON will look like this:
{ "output": [ { "type": "invoice", "invoiceNumber": "INV20023", "poNumber": 30278099, "amt": 100.5 }, { "type": "invoice", "invoiceNumber": "INV20024", "poNumber": 30288899, "amt": 50.99 } ] }
Feb 10, 2022
EDI platform
To support developers working with larger JSON documents, we have increased the maximum mapped document size from 1 megabyte to 4 megabytes in order to accommodate a wider range of use cases.
New $currentDateTime function in Mappings
You can now use $currentDateTime function to generate current date and time in different formats and timezones. For example, if you want to generate a current date in an EDI format, you can achieve this by $currentDateTime($dateTime.EDIDate). If you need to have it generated for a different timezone, you can do so by specifying the 2nd argument like so: $currentDateTime($dateTime.EDIDate, "Europe/Berlin"). Read more
Feb 9, 2022
EDI platform
Since launch, EDI Core served traffic from a single geographic region. Now, EDI Core serves traffic from multiple regions. This will increase the reliability of the service in the case of a regional outage, and decrease latency for requests made geographically closer.
Mappings: Lookup tables
You can now add one or more lookup tables to your mappings. Lookup tables are powerful for use cases where you have a field that contains a code and you wish to replace it with a related value.
For example, if you have a source field with a country code (`USA`) and you want to replace it with the country name (`United States`), you can achieve this by building a countries lookup table:

You can then use the lookup table in your mapping expression with the $lookupTable function:

To learn more, see: Mappings documentation, Mappings API documentation.
Feb 7, 2022
EDI platform
Now, when you explore an EDI file in Inspector, the Launch modal will generate a code snippet using that EDI payload.

Mappings: Ability to explicitly omit fields from the mapping output
Mappings now supports omitting fields from the mapping output using the $omitField constant.
If a given expression evaluates the $omitField constant, the field the expression is defined for will be omitted in the output. The $omitField constant is compatible with all mapping types and all JSONata expressions.
To learn more, refer to the Mappings documentation here.
Feb 1, 2022
EDI platform
We added a new Launch modal in Inspector with code snippets for making a HTTP request, cURL, Node.js + Axios, Python + Requests. Simply copy the code into a tool of your choice, insert your API key and a sample payload, and beging translating between EDI and JEDI programmatically.

Jan 31, 2022
EDI platform
EDI Inspector: ability to download EDI file and improved data rendering
You can now save an EDI file from the Inspector editor.
We also improved data rendering format making the EDI file more human-readable:
Dates previously displayed as 20210901 now are shown as Sep 1, 2021.
Prior to the change, X12 elements that had a paired relational constraint were displayed as two separate entries. Example:
Communication Number Qualifier: Internet Email Address <> EA Communication Number: team@stedi.com
We now combine these into a single entry, with the qualifier as the label. You can click on either of these values to see the relevant reference information.
Internet Email Address <> EA : team@stedi.com

EDI Reference: Human-readable conditions
The EDI Reference has been updated to display a human-readable interpretation of relation condition code (ex. P0304: If either PER-03 or PER-04 is present, then the other is required). Before the enhancement, only the relation condition code was provided, which was difficult to parse (ex. P0304).See example

Jan 20, 2022
EDI platform
When you create or import a mapping, you can now open a Launch modal with code snippets in cURL, Node.js + Axios, Python + Requests. Simply copy the code into a tool of your choice, insert your API key and a sample payload to try out the mapping.

EDI Core: format EDI files
You can now prettify unformatted EDI files in Inspector and through the /prettify endpoint.

Jan 12, 2022
EDI platform
You can now generate a sample EDI file from each and every transaction set on EDI Reference.

Jan 10, 2022
EDI platform
As a consumer of the /translate EDI core API, you now have the ability to parse EDI files that do NOT have envelopes. Before this enhancement, parsing a file without ISA/IEA GS/GE segments would result in a 422 response. Now, the EDI Core API will return a response based on the desired output parameters. The API response will identify the missing envelopes and elements for you.
View the response of the following payload in the inspector here:
ST*850*000000001~ BEG*24*SP*PO-00001**20210901~ N1*2L*STEDI INC.~ REF*K6*A composable platform for building flexible EDI systems~ PER*SR**EA*team@stedi.com~ PO1**1*2P*0.0001*PE*GE*EDI Core~ PO1**1*C0*0.05*PE*GE*Mappings~ CTT*2~ SE*9*000000001~
EDI Core: parse segments not in spec
The /translate EDI core API has been updated to support the parsing of segments that are not part of a given X12 release. Before this update, such a segment would result in a 422 response. Now, the API will return a valid response that clearly identifies the segment in question.
View the response of the following payload in the inspector here
ST*850*000000001~ BEG*24*SP*PO-00001**20210901~ N1*2L*STEDI INC.~ AUD*K6*<--AUD is NOT part of the 850 spec -->~ PER*SR**EA*team@stedi.com~ PO1**1*2P*0.0001*PE*GE*EDI Core~ PO1**1*C0*0.05*PE*GE*Mappings~ CTT*2~ SE*9*000000001~
Jan 7, 2022
EDI platform
You are now able to specify the option to remove_empty_segments in the output_options of the EDI Core API.
"output_options": { "generate_control_numbers": true, "remove_empty_segments": true },
This feature can be helpful in cases when you're translating from JEDI to EDI and you wish to omit blank segments. Read more
Announcing 98% price decrease for Mapping requests
As of January 1, 2022, Mapping has a new pricing table, seen here. The decreased price of $0.001 per request for new and existing customers costs 98% less than the previous price of $0.05 (for volumes between 101-1,000,000 requests a month).
The price per request is tiered and the first 100 requests per month are free.
Request CountPriceFirst 100FreeFrom 101 to 1,000,000$0.001Above 1,000,000Contact us
Jan 6, 2022
EDI platform
Until now, the new JEDI 2.0 format was in "beta" as it stabilized. As of today, JEDI 2.0 is now ready for production use and comes with long-term support and commitment to no breaking changes.
You can read more about the JEDI@2.0 format here.
Below is an example of a JEDI 2.0 file.
{ "interchanges": [ { "interchange_control_header_ISA": { "authorization_information_qualifier_01": "no_authorization_information_present_no_meaningful_information_in_i02_00", "authorization_information_02": "", "security_information_qualifier_03": "no_security_information_present_no_meaningful_information_in_i04_00", "security_information_04": "", "interchange_id_qualifier_05": "mutually_defined_ZZ", "interchange_sender_id_06": "", "interchange_id_qualifier_07": "mutually_defined_ZZ", "interchange_receiver_id_08": "", "interchange_date_09": "210902", "interchange_time_10": "1200", "repetition_separator_11": "/", "interchange_control_version_number_code_12": "00801", "interchange_control_number_13": "123456789", "acknowledgment_requested_code_14": "interchange_acknowledgment_requested_ta1_1", "interchange_usage_indicator_code_15": "test_data_T", "component_element_separator_16": ":" }, "groups": [ { "functional_group_header_GS": { "functional_identifier_code_01": "ocean_shipment_information_304_311_317_319_322_323_324_325_326_361_SO", "application_senders_code_02": "00", "application_receivers_code_03": "00", "date_04": "20210902", "time_05": "1200", "group_control_number_06": "987654321", "responsible_agency_code_07": "accredited_standards_committee_x12_X", "version_release_industry_identifier_code_08": "008010" }, "transaction_sets": [ { "heading": { "transaction_set_header_ST": { "transaction_set_identifier_code_01": "326", "transaction_set_control_number_02": "0000" }, "transaction_set_trailer_SE": { "number_of_included_segments_01": "2", "transaction_set_control_number_02": "0000" } }, "type": "326" } ], "functional_group_trailer_GE": { "number_of_transaction_sets_included_01": "1", "group_control_number_02": "987654321" } } ], "interchange_control_trailer_IEA": { "number_of_included_functional_groups_01": "1", "interchange_control_number_02": "123456789" }, "delimiters": { "element": "*", "segment": "~", "sub_element": ":", "repetition": "/" } } ] }
Jan 5, 2022
EDI platform
As of January 1, 2022, EDI Core has a new pricing table. The decreased price of $0.0075 per request for new and existing customers costs 85% less than the previous price of $0.05 (for volumes between 101-1,000,000 request a month).
The price per request is tiered and the first 100 requests per month are free.
Request CountPriceFirst 100FreeFrom 101 to 1,000,000$0.00750Above 1,000,000Contact us
API bytes processed per request pricing
The price per KiB is a flat 0.00005 per KiB.
KiBPrice1 KiB$0.00005
Mappings: "duplicate mapping" functionality
You are now able to duplicate an existing Mapping by clicking the "Duplicate" icon next to each Mapping in the Mappings list page:
Jan 1, 2022
EDI platform
EDI Reference provides users with comprehensive EDI documentation and X12 table data. Until now, Stedi only had support for all X12 table data from Version 4-8 (1998-present). Now, users who are still on older formats can access table data from Version 3 (003010 - 003070) dating back to 1991.
EDI Core's translate API enables users to translate between X12 and JEDI (JSON EDI), with validation against the specified release. Now, users can validate their X12 files against Version 3 releases using EDI Core.

Dec 23, 2021
EDI platform
You are now able to load a sample source/target JSON to quickly get started experimenting with Mappings. Until now, you had to provide your own JSON files to map.

Dec 14, 2021
EDI platform
Mappings now supports using the JSON array-of-objects structure as both source and target documents when building a mapping.
JSON documents converted from tabular data formats, like CSV, XML, etc., do not have a top-level object by default. Until now, it was impossible to set the list context correctly, without manually adding a top-level object.
With the expanded support of the JSON specification in Mappings, JSON array-of-objects structure can be used as the source and target documents, without the need for manual adjustments and additional transformations before and after the mapping request.
To learn more, refer to the JSONata array-of-objects cheatsheet here.
Dec 13, 2021
EDI platform
The following X12 EDI envelope trailers are now optional when converting JEDI 2.0 to EDI:
IEA GE SE LE
When these trailers are not included in the input JEDI, they are automatically generated based on the contents of the corresponding header and envelope. This simplifies the generation of EDI for users, as they can avoid potentially toilsome tasks such as counting the number of segments nested within a transaction set.

Dec 7, 2021
EDI platform
Mappings now has a $convertDateTime function which makes date formatting and parsing easier (see examples below). On top of that, Mappings now also provides $dateTime const with common date formats. See the documentation here
$convertDateTime("20140919", "yyyyMMdd", "yyyy-MM-dd") → "2014-09-19" $convertDateTime("2021-01-02T12:00:00Z", $dateTime.RFC3339, "yyyy-MM-dd") → "2021-01-02" $convertDateTime("2021-01-02T12:00:00+00:00", $dateTime.RFC3339, "yyyy-MM-dd") → "2021-01-02" $convertDateTime("210102", $dateTime.EDIDate, $dateTime.RFC3339) → "2021-01-02T12:00:00Z" $convertDateTime("12:00 2nd January 2021", "hh:mm do MMMM yyyy", "yyyy-MM-dd") → "2021-01-02"
Dec 6, 2021
EDI platform
Numbers stored in EDI may have adjustments applied to them based on how they're defined in a mapping guide. For instance, in an Invoice (810), you return the invoice's total not as 34.95, but as 3495. This field is noted as type "N2", meaning "this number has two decimal places."
With this change to JEDI@2.0-beta when using the EDI Core API, we handle the math for you - numbers provided with N types in the EDI will be converted to their real values in the JEDI document on the other end. Of course, if you translate JEDI to X12, we will handle this as well.
In the example below, we convert the 1450 in the SAC05 in the X12 on the left to 14.50 in the "amount_05" on the JEDI on the right.
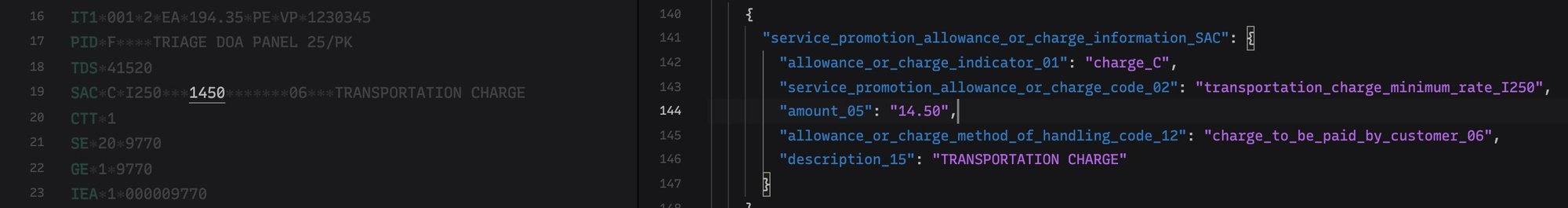
Dec 3, 2021
EDI platform
There is now an API to set the value of a control-number sequence for a specific sender+receiver pair.
The next generated control number will be the 1 + the value that you set. Control numbers roll back to 1 when reaching 1e9.
Inspector now supports JEDI 2.0 (Beta) and renders dates and times nicely
The Inspector now supports and displays JEDI@2.0-beta when viewing JSON.
We've also added custom renderers to nicely display dates and times, as well as numeric and decimal data types into the "rich view" of the Inspector.
EDI Core accepted codes list
There is a new output option to include_accepted_code_list for Jedi@1.0 and Jedi@2.0-beta. If enabled, a list of accepted_codes will be returned in the validation errors. This is disabled by default. This will help provide clearer error/validation messages. As an example of a validation error result:
{ "code": "invalid_id", "message": "Invalid code value 'X' specified for element N1-01", "path": [ "interchanges", "0", "groups", ... ], "severity": "error", "accepted_codes": [ "01", "02", "03", ... ] }
New homepage for EDI Reference
/edi has a brand new homepage. There you can search for any Element, Segment or Transaction Set and you can also see all the available X12 releases we have on the site.

Nov 30, 2021
EDI platform
In many mapping scenarios, a source document might contain one or more JSON arrays. In order to map an array like that to a different array on the target document, you need to specify a list context (see Mapping Loops).
Previously, you could only loop over all items on the source array and map each item, but it was not possible to change the order of the array elements or exclude certain array items from the result.
Today, we are adding support for JSONata functions usage when setting a List Context. With the support from $filter, $sort, $reverse, and other functions you should be able to translate an array of any shape to the desired format.
For example, assuming that the orders below are coming in a random sorting order, you can adjust that order and sort the result by orderDate before mapping them to shipments:
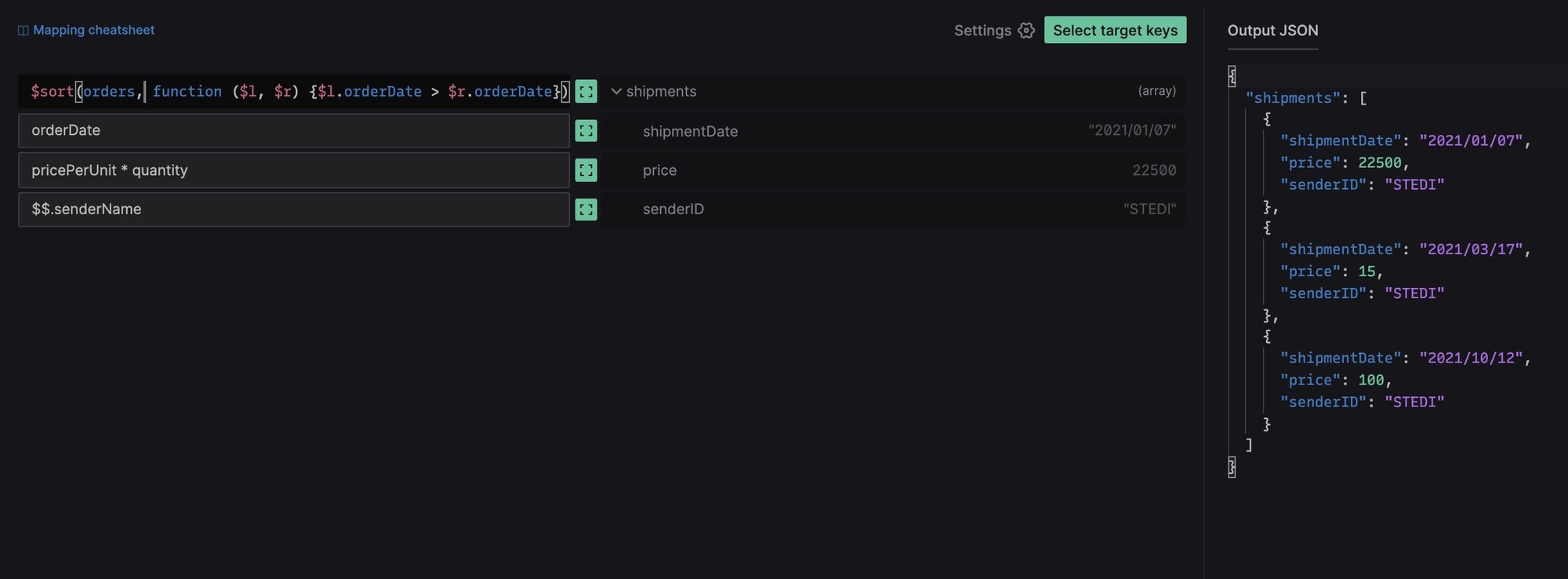
Nov 25, 2021
EDI platform
In addition to a friendly prompt to save your changes when leaving the Edit Mapping page, we've started to preserve unsaved changes in Local Storage inside the browser to further reduce the risk of losing any unfinished state of a mapping session.
Now, if you've spent a few hours building or editing a mapping, but you're not ready to submit the changes yet, you can leave the website and get an option to restore your in-progress state when you return to the same mapping.

It is important to note that only the last mapping session gets stored in Local Storage, so if you have multiple mappings to edit simultaneously, it is still advised to save your changes before closing the browser tab.
Nov 23, 2021
EDI platform
Mappings is a powerful, highly-available service built to create, test and run mappings between various JSON documents – from simple value-to-value data mapping to highly complex data transformations.
For the last 50 years, businesses across all industries have been utilizing EDI to send and receive commercial transactions like purchase orders and invoices with their trading partners. Given the immense range of available standards, data formats, and API shapes, mappings between input and output files are necessary. However, existing mapping tools are lagging behind modern software tooling in terms of API-driven accessibility, scalability, high-availability, and user experience. A large portion of these systems live on-prem, and are only accessible via legacy interfaces and protocols – making it hard to integrate with today’s software solutions.
For example, let's say you have a document that looks like this
{ "product": { "id": "QL-5490S", "price": "USD 500" } }
but you need it to look like this
{ "product_number": "QL-5490S", "price": { "currency": "USD", "amount": 500 } }
then Mappings can help you. Once you've created the proper mapping rules, Mappings can turn any document with the first structure into a document with the second structure. There are many situations where this is helpful, including:
You receive data from a trading partner, but it's not in the format that your own software system can handle.
You need to call an API and it expects data in a format that's different than what your own software system uses.
You want to map the data on a purchase order directly onto an invoice.
There are no minimums, monthly fees, or setup fees to use Mappings – customers only pay for the number of times their mapping is executed, starting at $0.05 per request. The first 100 requests per month are free.
To get started building Mappings, please visit terminal.stedi.com/mappings.
Nov 19, 2021
EDI platform
We released the second major revision of the JEDI format as a beta this week. This gives us some major readability gains over the original JEDI format, including:
We present the names of segments in addition to their IDs, so you have some context as to what each segment is representing
Similarly, we have added element descriptions along with their position in the segment
We also have updated how code values are provided/returned, with the codes being expanded to their representative text. We call out structural pieces of the document as well - loops are identified by the first segment of the loop (where jedi@1.0 sometimes had reference names that were just a numerical string), and each loop is designated with a _loop suffix.
We've added a couple of convenience attributes to the documents, so now you have an easier property on which to identify release and transaction set for a given document (at interchanges.*.release and interchanges.*.groups.*.transaction_set)
By default, we are trimming ISA header whitespace, but by supplying the clean_envelope_whitespace: false flag, this can be disabled. This differs from JEDi@1.0 which has this feature off by default. We're also still in beta, so we may make further tweaks and adjustments as time goes on, based on customer input and how people are using the documents. Please send us your feedback!
Compressed Response
Translating EDI to JEDI2.0 results in a much larger payload than the original request (and larger than the existing JEDI1.0 format). Now we compress all responses (larger than 5.5 kb) from the API. This compression is transparent to the customer as most http request clients and all browsers will decompress the response for them.
Oct 27, 2021
EDI platform
In order to make JEDI easier to read when it returns from our /translate endpoint, we have applied a custom sorting to the JSON renderer. JEDI will now order JEDI as the segments and elements are ordered in EDI. The order be will be preserved in node or browser applications. Other platforms may not keep the key ordering.
{ "interchanges": [ { "ISA": { "01": "00", "02": " " }, "groups": [ { "GS": { "01": "PO", "02": "SENDERGS", "08": "004010" }, "transaction_sets": [ { "heading": { "010_ST": { "01": "850", "02": "000000001" }, "020_BEG": { "01": "00", "02": "SA", "03": "A99999-01", "05": "19970214" } }, "detail": {}, "summary": {} } ], "GE": { "01": "1", "02": "1" } } ], "IEA": { "01": "1", "02": "000000001" }, "delimiters": { "element": "*", "segment": "~", "sub_element": ">" } } ] }
__version field in JEDI documents
To distinguish between versions of JEDI documents, we've added an attribute called __version to the response of /translate.
{ "code": "valid", "output": { "__version": "jedi@1.0", "interchanges": {...}, "meta": {...}, }, }
Trimmed ISA white space in JEDI documents
Added new output option to trim the ISA whitespace if enabled. Today, the ISA in JEDI format looks like
"ISA": { "01": "00", "02": " ", "03": "00", "04": " ", "05": "ZZ", "06": "TCWDEPOT ", "07": "ZZ", "08": "FVLI0006 ", "09": "210202", "10": "0235", "11": "U", "12": "00200", "13": "005787399", "14": "0", "15": "P", "16": ":" }
If clean_envelope_whitespace is set to true, it instead outputs as:
"ISA": { "01": "00", "02": "", "03": "00", "04": "", "05": "ZZ", "06": "TCWDEPOT", "07": "ZZ", "08": "FVLI0006", "09": "210202", "10": "0235", "11": "U", "12": "00200", "13": "005787399", "14": "0", "15": "P", "16": ":", }
JSON EDI view in the Inspector
You can now toggle between "Rich view" and "JSON view" in the Inspector. The JSON view displays the EDI input in our custom JSON EDI (JEDI for short) format, along with the same annotations that were present in Terminal, for faster manual scanning of the file.

Support missing X12 003XXX versions
Support for 003040 and 003030 are now visible from our EDI Reference. More to come.
Faster EDI Inspector experience on the web
A missing header on responses from EDI Core meant that browsers would always need to issue two synchronous requests in order to translate and validate payloads in EDI Inspector. The addition of the missing headers speeds up the experience considerably, especially for users far away from Virginia, USA.
Oct 19, 2021
EDI platform
To improve the legibility of JEDI v1 in Terminal, a description was added next to each segment and element.
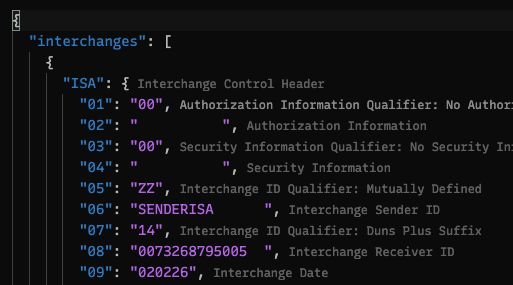
ISA segment padding
The ISA segment of an X12 EDI document has fixed width fields for each element so the length of the segment always turns out the exact same length. Previously, converting from JEDI to EDI required that ISA elements be of accurate length.
X12 3XXX releases
Support for 3050, 3060, and 3070 X12 releases has been added to EDI Reference and EDI Core's /translate endpoint.
