Submit professional claims
You can send 837P professional claims to payers through the Stedi portal, the Professional Claims API, or an SFTP connection.
Once you send a claim, Stedi automatically receives and processes 277CA claim acknowledgment and 835 Electronic Remittance Advice (ERA) responses.
Before sending claims
You may need to complete the following steps before sending claims.
Transaction enrollment
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. Some payers require enrollment before allowing providers to submit 837 claims through a new clearinghouse.
Enrolling through Stedi may cancel existing claims enrollments you have through other clearinghouses. We can help you determine whether this applies to your specific payers. However, enrolling through Stedi for 837 claims doesn't affect your existing enrollments for other transaction types. For example, enrolling with Stedi won't unenroll the provider from receiving transactions like Electronic Remittance Advices (ERAs) through other clearinghouses.
You can check whether a specific payer requires transaction enrollment for 837 claims in the Payer Network or through the Payers API.
To enroll, complete the following steps:
- Create a provider record with the information required for enrollment. If you already have a record for the provider, you can skip this step. Stedi portal | API endpoint
- Submit an enrollment request for the claim type. Stedi portal | API endpoint
Coordination of benefits check
We recommend running a coordination of benefits (COB) check to ensure you submit claims to the correct payer. COB checks can help you determine:
- If a patient is covered by more than one health plan
- Whether coverage overlap requires coordination of benefits
- Each payer’s responsibility for payment (primacy) in coordination of benefits scenarios
Visit Coordination of benefits (COB) checks for more information.
UI submission
You can submit professional claims through the Stedi portal. Manual claim submission can be useful for testing, QA, and debugging your pipeline.
You can submit professional claims either through our interactive claim form or by uploading X12 EDI claim data.
CMS-1500 claim form
You can only submit claims to the patient's primary health plan through our interactive CMS-1500 form. You must submit secondary or tertiary claims through X12 EDI upload, API, or SFTP instead.
To submit a professional claim, do one of the following:
- Go to the Transactions page and click + Submit claim manually.
- Go to the Claims menu and select + Submit claim.
The submission form is based on the CMS-1500 Claim Form.
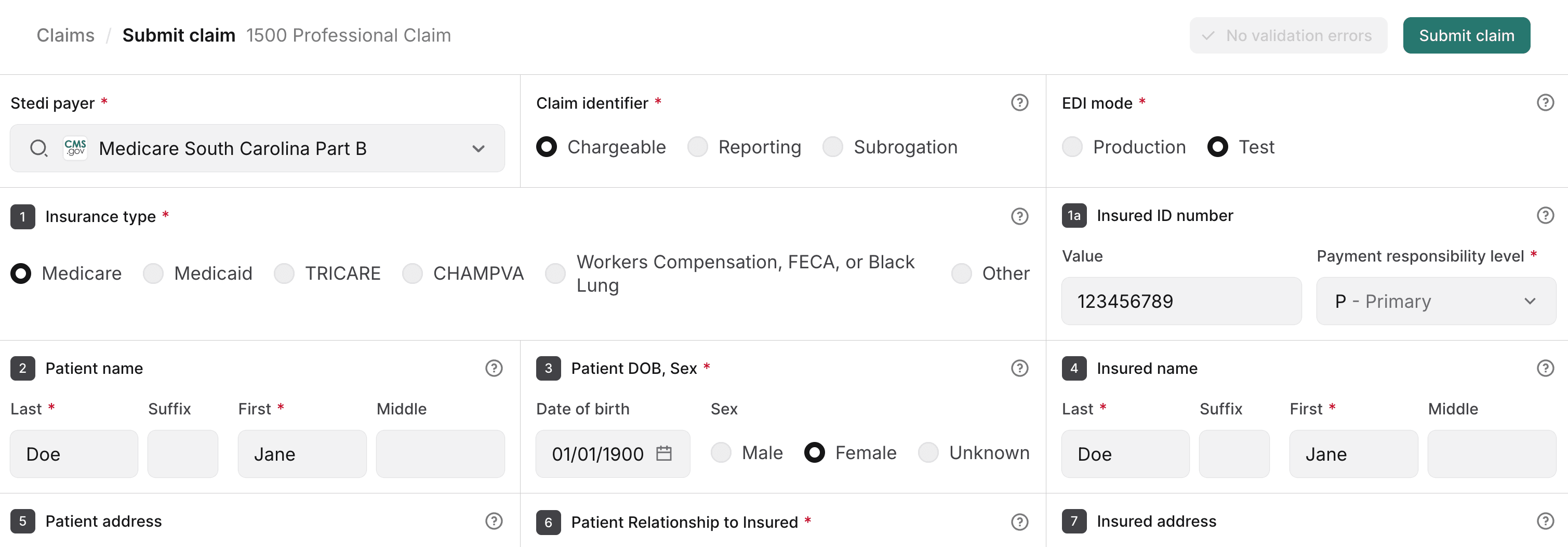
Enter the required information for your professional claim. Notably:
- Select a Payer from the dropdown list. Start typing to filter the list.
- Select whether you want to submit a Production or Test claim.
- Production claims are sent to the payer.
- Test claims aren't sent to the payer. Stedi validates them and displays them in the portal so you can get familiar with Stedi's claim processing workflow. Stedi responds to test claims with a 277CA claim acknowledgment, but you won't receive an 835 Electronic Remittance Advice (ERA).
- We strongly recommend submitting a unique value for the Patient account number. The identifier should be more complex than a simple sequential number and should be hard to guess. The payer returns this value in related transactions, such as the 277CA and 835 ERA, so you can correlate responses and real-time claim status checks with the original claim.
- Keep it 17 characters or less. Some payers cut off values longer than 17 characters in ERAs and claim acknowledgments, which makes it hard to match them with the original claim.
- Use alphanumeric characters only. Avoid special characters, as many payers don't handle them properly.
- Use random strings. Formats with patient initials or the date of service in them can create duplicates.
- You can submit claim-level attachments in Box 19 and service-line attachments in Box 24 - Service lines. Note that you can't add attachments to claims that were already submitted through the portal. To include attachments for those, resubmit the claim with the attachments.
- Click Add attachment to specify the details for an attachment.
- Choose the appropriate Report type for each attachment.
- Choose the appropriate Transmission code. If you plan to upload an attachment file, set this to EL (EDI). If you plan to submit the attachment through another method, such as directly through the payer's portal, set this to the appropriate code.
- Either enter the Attachment control number or click Upload file to select the file you want to attach. Supported file types are JPG, PDF, PNG, or TIFF. Each attachment should be 10 MB or less to comply with most payer requirements. You can add up to 10 attachment files at the claim level and up to 10 attachment files for each service line. If you included attachment files, Stedi automatically generates the required attachment control numbers for you.
When you're finished, click Submit claim. Stedi validates the claim and submits it to the payer. It will appear on the Transactions page as a new 837P Professional Claim.
X12 EDI upload
Your X12 EDI claim data must adhere to the 837 Claim: Professional (X222A1) specification.
To manually submit an X12 EDI claim:
- Go to the Transactions page.
- Click Submit claim and choose Upload EDI file from the menu.
- Do one of the following:
- Click Upload X12 EDI and select an existing
.edifile to add. - Select the transaction type and then paste the X12 EDI content into the text area.
- Click Upload X12 EDI and select an existing
- Configure the settings to send a test or a production claim. Production claims are sent to payers. Test claims aren't sent to payers - Stedi's test clearinghouse processes them and returns test 277CA acknowledgments so you can evaluate your claim processing pipeline.
- Select either Test or Production in the menu at the top of the text area.
- Set
ISA15(Interchange Usage Indicator) toT(Test Data) orP(Production Data), accordingly.
- Fix any validation errors that appear after adding the claim X12 EDI content. Stedi highlights errors in red and displays the specification for the claim type you selected on the right side of the screen to make it easier to identify and fix issues.
- Click Submit claim to submit the claim to Stedi.
Stedi processes the claim and takes you to the claim's details page. Stedi also displays the claim on the Transactions page.
SFTP submission
You can use Stedi’s fully-managed SFTP server to submit claims to to payers and retrieve claim responses without calling Stedi’s APIs.
You must submit claims in X12 EDI format, and Stedi returns claim responses through the SFTP connection in X12 EDI format. This makes Stedi SFTP a good option if you have an existing system that generates X12 EDI files and you want to send them through the Stedi clearinghouse without completing an API integration. Visit SFTP connection for more information.
API submission
Call one of the following endpoints to submit 837P professional claims:
- Professional Claims to send requests in JSON
- Professional Claims Raw X12 to send requests in X12 EDI
Both endpoints return a synchronous response from Stedi in JSON format. Later, the payer will respond with a 277CA claim acknowledgment.
Headers
When constructing the request, you must include the following information in HTTP headers:
Authorization: Generate an API key to use for authentication.Content-Type: Set toapplication/json.
Body - JSON
The information you submit for a claim depends on your use case. Refer to the Professional Claims endpoint for a complete list of properties. However, all claims require the following high-level information:
| Information | Description |
|---|---|
tradingPartnerServiceId | This is the payer ID. You can send requests using the primary payer ID, the Stedi payer ID, or any alias listed in the payer record. If you don't already have payer IDs you use today, we recommend using the primary Payer ID. Visit the Payer Network for a complete list. |
tradingPartnerName | This is the payer's business name, like Cigna or Aetna. |
submitter object | Information about the entity submitting the claim. This can be either an individual or an organization, such as a doctor, hospital, or insurance company. |
receiver object | Information about the payer, such as an insurance company or government agency. |
subscriber and/or dependent objects | Information about the patient who received the medical services. Note that if a dependent has their own, unique member ID for their health plan, you should submit their information in the subscriber object and omit the dependent object from the request. You can check whether the dependent has a unique member ID by submitting an Eligibility Check to the payer for the dependent. The payer will return the member ID in the dependents.memberId field, if present. |
claimInformation object | Information about the claim, such as the patient control number, claim charge amount, and place of service code. It also includes information about each individual service line included in the claim. |
billing object | Information about the billing provider, such as the NPI, taxonomy code, and organization name. |
Patient Control Number
You must submit a Patient Control Number (PCN) with each claim in claimInformation.patientControlNumber. The payer returns this value in related transactions, such as the 277CA claim acknowledgment and 835 Electronic Remittance Advice (ERA), so you can correlate responses and real-time claim status checks with the original claim.
When assigning a PCN, follow these best practices:
- Use a unique PCN for each claim. The identifier should be more complex than a simple sequential number and should be hard to guess.
- Use random strings. Formats with patient initials or the date of service in them can create duplicates. We recommend using nanoid or a similar library to create a strong, unique 17-character PCN for each claim.
- Keep it 17 characters or less. Some payers cut off values longer than 17 characters in ERAs and claim acknowledgments, which makes it hard to match them with the original claim.
- Use alphanumeric characters only. Avoid special characters, as many payers don't handle them properly.
Service line identification
A claim can contain multiple service lines. Since the payer may accept, reject, or pay a subset of those lines, you can receive an 835 ERA that references a patientControlNumber, but only pertains to some of the service lines.
However, the claimInformation.serviceLines.providerControlNumber serves as a unique identifier for each service line in your claim submission. This value appears in the 277CA claim acknowledgment and 835 ERA as the lineItemControlNumber, allowing you to correlate these responses to specific service lines from the original claim. If you don't set the providerControlNumber for a service line, Stedi uses a random UUID.
Stedi returns service line identifiers in the claimReference.serviceLines object of the synchronous API response.
Conditional requirements
Note that objects marked as required are required for all requests, while others are conditionally required depending on the circumstances. When you include a conditionally required object, you must include all of its required properties.
For example, you must always include the subscriber object in your request, but you only need to include the supervising object when the rendering provider is supervised by a physician.
Body - X12 EDI
You must send a payload in 837 X12 EDI format.
Note the following requirements and behavior when sending professional claims through the raw X12 endpoint.
Envelope and header
Stedi generates its own ISA and GS headers and IEA and GE trailers before sending your claim to the payer. You can submit your claim to Stedi with any values in these segments, as long as they conform to the X12 EDI specification.
However, you must set ST03 (Implementation Guide Version Name) to 005010X222A1.
Payer ID
You must submit a payer identifier in Loop 2010BB (Payer Name) NM109 so Stedi can route your claim to the correct payer. This identifier must be a payer ID or payer ID alias listed in the Payer Network. If you don't already have payer IDs you use today, we recommend using the primary Payer ID.
CLM01 (Patient Control Number)
We strongly recommend submitting a unique value for Loop 2300 (Claim Information) CLM01 (Patient Control Number). The payer returns this value in related transactions, such as the 277CA claim acknowledgment and 835 Electronic Remittance Advice (ERA), so you can correlate responses and real-time claim status checks with the original claim.
When assigning a PCN, follow these best practices:
- Use a unique PCN for each claim. The identifier should be more complex than a simple sequential number and should be hard to guess.
- Use random strings. Formats with patient initials or the date of service in them can create duplicates. We recommend using nanoid or a similar library to create a strong, unique 17-character PCN for each claim.
- Keep it 17 characters or less. Some payers cut off values longer than 17 characters in ERAs and claim acknowledgments, which makes it hard to match them with the original claim.
- Use alphanumeric characters only. Avoid special characters, as many payers don't handle them properly.
Service line identification
A claim can contain multiple service lines. Since the payer may accept, reject, or pay a subset of those lines, you can receive an 835 response that references a patient control number, but only pertains to some of the service lines.
However, the line item control number serves as a unique identifier for each service line in your claim submission.
- You can set the line item control number in
Loop 2400 REF02, whenREF01=6R. The line item control number appears in the 277CA and 835 ERA responses as thelineItemControlNumber, allowing you to correlate these responses to specific service lines from the original claim. - If you don’t set the line item control number for a service line, Stedi uses a ULID.
Character restrictions
Only use the X12 Basic and Extended character sets in request data. Using characters outside these sets may cause validation and HTTP 400 errors.
In addition, the following characters are reserved for delimiters in the final X12 EDI transaction to the payer: ~, *, :, and ^. X12 doesn’t support using escape sequences to represent delimiters or special characters. Stedi returns a 400 error if you use these restricted characters improperly.
- JSON endpoint: Don’t include delimiter characters anywhere in your request data.
- Raw X12 endpoint: You can use these characters as delimiters, but not in the body of the request data.
Sample request and response
The following examples send a professional claim. The response shape is the same for both the JSON and X12 EDI endpoints. It contains summary information from Stedi about the claim submission and whether it was successful.
curl --request POST \
--url https://healthcare.us.stedi.com/2024-04-01/change/medicalnetwork/professionalclaims/v3/submission \
--header 'Authorization: <api-key>' \
--header 'Content-Type: application/json' \
--data '{
"usageIndicator": "T",
"tradingPartnerServiceId": "6400",
"submitter": {
"organizationName": "Test Data Health Services, Inc.",
"submitterIdentification": "<YOUR-SUBMITTER-ID>",
"contactInformation": {
"name": "Test Data Health Services, Inc.",
"phoneNumber": "5552223333"
}
},
"receiver": {
"organizationName": "Cigna"
},
"subscriber": {
"memberId": "U7777788888",
"paymentResponsibilityLevelCode": "P",
"subscriberGroupName": "Cigna",
"firstName": "John",
"lastName": "Anon",
"gender": "M",
"dateOfBirth": "20000101",
"groupNumber": "3335555",
"address": {
"address1": "2222 Random St",
"city": "A City",
"state": "NY",
"postalCode": "123450000"
}
},
"billing": {
"providerType": "BillingProvider",
"npi": "<YOUR-BILLING-PROVIDER-NPI>",
"employerId": "123456789",
"taxonomyCode": "2084P0800X",
"organizationName": "Therapy Associates",
"address": {
"address1": "123 Some St",
"address2": "Floor 1",
"city": "A City",
"state": "NY",
"postalCode": "123450000"
},
"contactInformation": {
"name": "Test Data Health Services, Inc.",
"phoneNumber": "5553334444"
}
},
"claimInformation": {
"claimFilingCode": "CI",
"patientControlNumber": "<YOUR-CLAIM-ID>",
"claimChargeAmount": "109.20",
"placeOfServiceCode": "02",
"claimFrequencyCode": "1",
"signatureIndicator": "Y",
"planParticipationCode": "A",
"benefitsAssignmentCertificationIndicator": "Y",
"releaseInformationCode": "Y",
"healthCareCodeInformation": [
{
"diagnosisTypeCode": "ABK",
"diagnosisCode": "F1111"
}
],
"serviceFacilityLocation": {
"organizationName": "Smith Associates",
"address": {
"address1": "1234 Other St",
"city": "A City",
"state": "NY",
"postalCode": "123450000"
},
"npi": "1999999984"
},
"serviceLines": [
{
"serviceDate": "20240101",
"professionalService": {
"procedureIdentifier": "HC",
"procedureCode": "90837",
"procedureModifiers": [
"95"
],
"lineItemChargeAmount": "109.20",
"measurementUnit": "UN",
"serviceUnitCount": "1",
"compositeDiagnosisCodePointers": {
"diagnosisCodePointers": [
"1"
]
}
},
"providerControlNumber": "111222333",
"renderingProvider": {
"providerType": "RenderingProvider",
"npi": "<YOUR-PROVIDER-NPI>",
"taxonomyCode": "111YP2000X",
"firstName": "Jane",
"lastName": "Smith"
}
}
]
},
"tradingPartnerName": "Cigna"
}'curl --request POST \
--url https://healthcare.us.stedi.com/2024-04-01/change/medicalnetwork/professionalclaims/v3/raw-x12-submission \
--header 'Authorization: <api-key>' \
--header 'Content-Type: application/json' \
--data '{
"x12": "ISA*00* *00* *ZZ*001690149382 *ZZ*STEDITEST *240630*0847*^*00501*000000001*0*T*>~GS*HC*001690149382*STEDITEST*20240630*084744*000000001*X*005010X222A1~ST*837*0001*005010X222A1~BHT*0019*00*01J1M588QT2TAV2N093GNJ998T*20240630*0847*CH~NM1*41*2*Test Data Health Services, Inc.*****46*123567890~PER*IC*Test Data Health Services, Inc.*TE*5552223333~NM1*40*2*Cigna*****46*60054~HL*1**20*1~PRV*BI*PXC*2084P0800X~NM1*85*2*Therapy Associates*****XX*1999999984~N3*123 Some St*Floor 1~N4*A City*NY*123450000~REF*EI*832675429~PER*IC*Test Data Health Services, Inc.*TE*5553334444~HL*2*1*22*0~SBR*P*18*3335555******CI~NM1*IL*1*Anon*John****MI*U7777788888~N3*2222 Random St~N4*A City*NY*123450000~DMG*D8*20000101*M~NM1*PR*2*Cigna*****PI*60054~CLM*22266555*109.0***02>B>1*Y*A*Y*Y~HI*ABK>F1111~NM1*82*1*Smith*Jane****XX*1999999984~PRV*PE*PXC*111YP2000X~NM1*77*2*Smith Associates*****XX*1999999984~N3*1234 Other St~N4*A City*NY*123450000~LX*1~SV1*HC>90837>95*109.2*UN*1.0***1~DTP*472*D8*20240101~SE*30*0001~GE*1*000000001~IEA*1*000000001~"
}'{
"status": "SUCCESS",
"controlNumber": "555123",
"tradingPartnerServiceId": "6400",
"claimReference": {
"correlationId": "01HTQX03MMP4XHBT4QBGDAD9DG",
"patientControlNumber": "22266555",
"timeOfResponse": "2024-04-05T19:50:34.275Z",
"payerId": "6400",
"formatVersion": "5010",
"rhclaimNumber": "01HTQX03MMP4XHBT4QBGDAD9DG"
},
"httpStatusCode": "200 OK",
"meta": {
"traceId": "bef31123-34d8-46b6-b1ff-2a534d0e9a06"
},
"payer": {
"payerName": "Cigna",
"payerId": "6400"
}
}Test claims
All claims you submit through the API are sent to the payer as production claims unless you explicitly designate them as test data.
To send test claims:
- JSON endpoint: Set the
usageIndicatorproperty in the test claim body toT. - X12 EDI endpoint: Set
ISA15(Interchange Usage Indicator) toT(Test Data) instead ofP(Production Data).
When you send a test claim, Stedi doesn't send it to the payer. Instead, it processes the claim as if it were sent to the payer and returns a 277CA claim acknowledgment indicating whether the claim was successfully processed. Designating a claim as test data also allows you to filter for test claims on the Transactions page in the Stedi portal.
You'll receive a 277CA claim acknowledgment in response to test claims, but you won't receive a test 835 Electronic Remittance Advice (ERA) response unless you send the claim to the Stedi Test Payer. Visit Test claims workflow to learn how generate test ERAs.
Concurrency limit
Professional claim submission endpoints share a concurrency pool with other claim endpoints. For more information, visit Concurrency limits.
Recommended API clients
You may want to use an API client to make testing and debugging easier.
We don't recommend using Postman for requests containing Protected Health Information (PHI) because Postman defaults to storing request history - including full request payloads - on its cloud servers. You can’t turn this feature off without impractical workarounds.
Visit API clients for a list of recommended clients you can use instead.
View submitted claims
You can view the files that Stedi sends and receives on the Files page of the Stedi portal.
On the Transactions page, you can review and filter claims by Usage - production or test. Click any claim submission to review its details, including the full request and response payload, processing events, and a link to download the auto-generated 1500 Claim Form PDF.
275 claim attachments
If the claim requires attachments, you must include additional details about the attachments in the appropriate objects:
- Attachments for entire claim:
claimInformation.claimSupplementalInformation.reportInformationorclaimInformation.claimSupplementalInformation.reportInformations(multiple attachments) - Attachments for a specific service line:
claimInformation.serviceLines.serviceLineSupplementalInformation
Visit Claim attachments for complete instructions.
Submit to a secondary or tertiary payer
In coordination of benefits (COB) scenarios, you'll need to submit a claim to multiple payers.
You must set the subscriber.paymentResponsibilityLevelCode to either S (when submitting to the secondary payer) or T (when submitting to the tertiary payer).
You must also include the following information about how prior payers have adjudicated the claim. For example, if a patient's private insurance plan (primary payer) adjusted the requested reimbursement amount and paid for its portion of the services, you must include that information in the claim you submit to Medicare (secondary payer). You can find these details in 835 ERA responses from prior payers.
Claim information
You must submit one claimInformation.otherSubscriberInformation object for each prior payer. Supply all the required properties in the object plus the following additional information:
claimLevelAdjustments: Provide if the prior payer made adjustments at the claim level. Codes and their associated amounts must come from ERAs sent by the prior payers. You can find these codes in the ERA'stransactions.detailInfo.paymentInfo.claimAdjustmentsobject.medicareInpatientAdjudication(institutional claims only): You must include this if Medicare was one of the prior payers and reported inpatient adjudication information on the ERA.medicareOutpatientAdjudication: You must include this if Medicare was one of the prior payers and reported outpatient adjudication information on the ERA.otherPayerName.otherPayerAdjudicationOrPaymentDate: The date the payer adjudicated or paid the claim. You must provide this if you aren't providing a value in theclaimInformation.serviceLines.lineAdjudicationInformation.adjudicationOrPaymentDateproperty.payerPaidAmount: This is the total amount in dollars the payer paid on this claim.
Service line information
You must submit serviceLines.lineAdjudicationInformation objects when the prior payers provided line-level adjudication information. Submit one object for each prior payer. For each object, you should include the following properties.
adjudicationOrPaymentDate: The date the payer adjudicated or paid the claim. Don't include this if you're providing a date in theotherPayerName.otherPayerAdjudicationOrPaymentDateproperty.claimAdjustmentInformation: You can find this information in the ERA'stransactions.detailInfo.paymentInfo.serviceLines.serviceAdjustmentsobject.otherPayerPrimaryIdentifier: The identifier for the other payer. This value should match the identifier you supplied for the payer in theclaimInformation.otherSubscriberInformation.otherPayerName.otherPayerIdentifierproperty.procedureCode: The adjudicated procedure code for the service line.serviceIdQualifier: A code identify the type of procedure code. Visit Claims code lists for a complete list.serviceLinePaidAmount: The total amount in dollars the prior payer paid on this service line.paidServiceUnitCount: The number of paid units for the service line. When paid units are not present on the remittance advice, use the original billed units.remainingPatientLiability: The amount of the service line the patient is responsible for paying.
Claim Filing Indicator Code
The Claim Filing Indicator Code indicates how a claim was filed with a payer, such as MC (Medicaid) or CI (Commercial Insurance Co.).
Choosing the correct claim filing indicator code is important for successful claim submission. Visit the Claims code lists documentation for best practices for selecting the appropriate code.
Set a claim's correlation ID
A claim's correlation ID is a business identifier that you can use to track and manage claims.
- When you submit claims through the JSON endpoint, Stedi generates the correlation ID for you, and this value will be unique for each claim.
- When you submit claims in X12 EDI through the API or an SFTP connection, you can specify your own correlation ID in the
BHT03element. This allows you to use the same value for multiple claims if desired.
CMS-1500 claim form PDF
Stedi automatically generates a PDF CMS-1500 claim form for each professional claim you submit. You can manually download the form on the transaction details page for the claim in the Stedi portal or retrieve them programmatically through the following endpoints:
- CMS-1500 PDF: Business Identifier: Retrieve PDFs through a claim's business identifier. You can find the business identifier value in the
claimReference.correlationIdproperty Stedi returns in the synchronous claim submission response. - CMS-1500 PDF: Transaction ID
: Retrieve PDFs through the
transactionIdStedi assigns to the processed claim. This ID is included in the transaction processed event for the claim, which you can receive automatically through webhooks. You can also retrieve this ID from the transaction's details page in Stedi.
Payers have strict requirements for submitted CMS-1500 claim forms. If you plan to send generated PDFs to payers or retain them for your records, we strongly recommend visiting CMS-1500 Claim Form PDF for information about how to structure claim submissions for optimal generation, the correct printer settings for generated PDFs, and general best practices.