CMS now requires attestation for Medicare eligibility checks
Feb 17, 2026
Eligibility checks
To run Medicare eligibility checks with CMS, providers must complete an attestation by May 11, 2026.
Without attestation, CMS will reject Medicare eligibility requests for the provider starting on or after May 11, 2026.
What's changing
The Centers for Medicare and Medicaid Services (CMS) now requires providers to attest that clearinghouses – like Stedi – are allowed to run Medicare eligibility checks on their behalf. CMS also refers to this attestation as HETS EDI Enrollment.
This applies to all CMS trading partners, not just Stedi.
Stedi is updating new and existing CMS eligibility enrollments to include a required attestation step.
To avoid disruption to Medicare eligibility checks, attestation must be completed by May 11, 2026.
Important: The requirement doesn’t apply to:
Medicare Advantage, also called Medicare Part C
Medicare Part D
Existing enrollments
On February 17, 2026, Stedi moved any existing CMS eligibility check enrollments without an attestation to an enrollment status of PROVIDER_ACTION_REQUIRED. These enrollments now include a task with instructions to complete attestation.
Stedi also sent a notification email to the address in the enrollment's userEmail field (called Person for Stedi to contact in the Stedi portal). The email includes a link to the enrollment.
After the provider completes attestation and you mark the related enrollment task as complete, Stedi will move the CMS enrollment to the LIVE status.
How to find affected enrollments
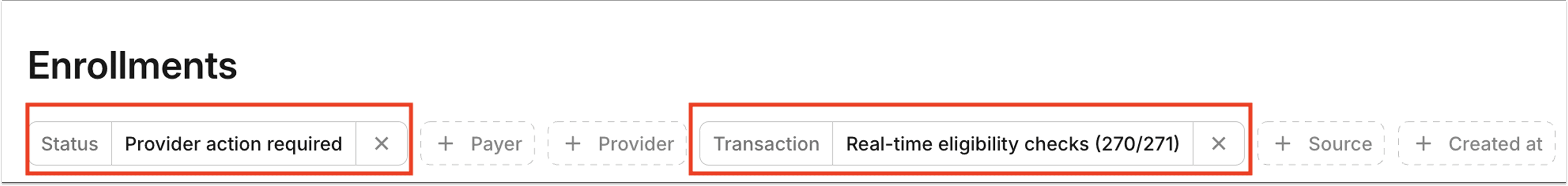
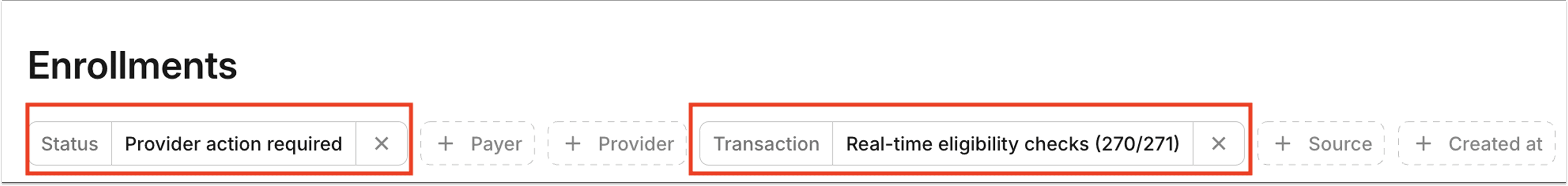
To view these enrollments in the Stedi portal, filter for a Status of Provider Action Required and Transaction of Real-time eligibility checks (270/271) on the Enrollments page:
You can also retrieve the enrollments using the following query parameters for the List Enrollments API endpoint:
curl --request GET \ --url "https://enrollments.us.stedi.com/2024-09-01/enrollments?status=PROVIDER_ACTION_REQUIRED&transactions=eligibilityCheck" \ --header "Authorization: <api_key>"
New enrollments
Starting February 16, 2026, new CMS eligibility check enrollments will require attestation. The process works as follows:
When you submit a CMS eligibility check enrollment request, Stedi moves its status to
STEDI_ACTION_REQUIRED.Stedi submits your enrollment to CMS within 1-2 business days.
After submitting your enrollment to CMS, Stedi moves the enrollment to the
PROVIDER_ACTION_REQUIREDstatus and adds an enrollment task to complete attestation.After the provider completes attestation and you mark the related enrollment task as complete, Stedi moves the enrollment to the
LIVEstatus.
Note: Once attestation is complete, you can run CMS eligibility checks immediately, even if the enrollment status is not yetLIVE.
Automatic enrollment requests for CMS
If a CMS eligibility check returns AAA error 41 (Authorization/Access Restrictions), indicating the provider is not enrolled for eligibility checks with CMS, Stedi automatically submits a CMS eligibility enrollment request for that provider.
Starting February 16, 2026, these automatic enrollment requests will follow the process for new CMS eligibility enrollments described above and require provider attestation. Previously, Stedi completed these enrollments without requiring provider action.
This feature was previously called “automatic enrollment.” We're now calling it “automatic enrollment requests.”
How to complete attestation
Attestation must be completed for each billing National Provider Identifier (NPI) enrolled with CMS for eligibility checks. There is no bulk attestation across NPIs.
Stedi can't complete this step on the provider’s behalf.
Stedi provides a task and instructions for completing the CMS attestation in:
The Tasks section of the enrollment request's details page in the Stedi portal.
The
tasksobject array of the List Enrollments and Retrieve Enrollment API responses.
You can also view the instructions in our Transaction Enrollments Hub.
How long does attestation take?
Attestation takes approximately 5-15 minutes to complete per NPI.
Timing
CMS has stated they'll enforce attestation requirements on May 11, 2026.
When enforcement begins, CMS will return AAA error 41 (Authorization/Access Restrictions) for Medicare eligibility checks with an NPI that has not completed attestation.
Until then, Medicare eligibility checks will continue to work as normal.
Support
If you have questions or concerns, contact us using your dedicated support channel or our contact form.
To run Medicare eligibility checks with CMS, providers must complete an attestation by May 11, 2026.
Without attestation, CMS will reject Medicare eligibility requests for the provider starting on or after May 11, 2026.
What's changing
The Centers for Medicare and Medicaid Services (CMS) now requires providers to attest that clearinghouses – like Stedi – are allowed to run Medicare eligibility checks on their behalf. CMS also refers to this attestation as HETS EDI Enrollment.
This applies to all CMS trading partners, not just Stedi.
Stedi is updating new and existing CMS eligibility enrollments to include a required attestation step.
To avoid disruption to Medicare eligibility checks, attestation must be completed by May 11, 2026.
Important: The requirement doesn’t apply to:
Medicare Advantage, also called Medicare Part C
Medicare Part D
Existing enrollments
On February 17, 2026, Stedi moved any existing CMS eligibility check enrollments without an attestation to an enrollment status of PROVIDER_ACTION_REQUIRED. These enrollments now include a task with instructions to complete attestation.
Stedi also sent a notification email to the address in the enrollment's userEmail field (called Person for Stedi to contact in the Stedi portal). The email includes a link to the enrollment.
After the provider completes attestation and you mark the related enrollment task as complete, Stedi will move the CMS enrollment to the LIVE status.
How to find affected enrollments
To view these enrollments in the Stedi portal, filter for a Status of Provider Action Required and Transaction of Real-time eligibility checks (270/271) on the Enrollments page:
You can also retrieve the enrollments using the following query parameters for the List Enrollments API endpoint:
curl --request GET \ --url "https://enrollments.us.stedi.com/2024-09-01/enrollments?status=PROVIDER_ACTION_REQUIRED&transactions=eligibilityCheck" \ --header "Authorization: <api_key>"
New enrollments
Starting February 16, 2026, new CMS eligibility check enrollments will require attestation. The process works as follows:
When you submit a CMS eligibility check enrollment request, Stedi moves its status to
STEDI_ACTION_REQUIRED.Stedi submits your enrollment to CMS within 1-2 business days.
After submitting your enrollment to CMS, Stedi moves the enrollment to the
PROVIDER_ACTION_REQUIREDstatus and adds an enrollment task to complete attestation.After the provider completes attestation and you mark the related enrollment task as complete, Stedi moves the enrollment to the
LIVEstatus.
Note: Once attestation is complete, you can run CMS eligibility checks immediately, even if the enrollment status is not yetLIVE.
Automatic enrollment requests for CMS
If a CMS eligibility check returns AAA error 41 (Authorization/Access Restrictions), indicating the provider is not enrolled for eligibility checks with CMS, Stedi automatically submits a CMS eligibility enrollment request for that provider.
Starting February 16, 2026, these automatic enrollment requests will follow the process for new CMS eligibility enrollments described above and require provider attestation. Previously, Stedi completed these enrollments without requiring provider action.
This feature was previously called “automatic enrollment.” We're now calling it “automatic enrollment requests.”
How to complete attestation
Attestation must be completed for each billing National Provider Identifier (NPI) enrolled with CMS for eligibility checks. There is no bulk attestation across NPIs.
Stedi can't complete this step on the provider’s behalf.
Stedi provides a task and instructions for completing the CMS attestation in:
The Tasks section of the enrollment request's details page in the Stedi portal.
The
tasksobject array of the List Enrollments and Retrieve Enrollment API responses.
You can also view the instructions in our Transaction Enrollments Hub.
How long does attestation take?
Attestation takes approximately 5-15 minutes to complete per NPI.
Timing
CMS has stated they'll enforce attestation requirements on May 11, 2026.
When enforcement begins, CMS will return AAA error 41 (Authorization/Access Restrictions) for Medicare eligibility checks with an NPI that has not completed attestation.
Until then, Medicare eligibility checks will continue to work as normal.
Support
If you have questions or concerns, contact us using your dedicated support channel or our contact form.
Get started with Stedi
Get started with Stedi
Automate healthcare transactions with developer-friendly APIs that support thousands of payers. Contact us to learn more and speak to the team.
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Developers
Resources
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Developers
Resources
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Developers
Resources
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
