277CA claim acknowledgments
You may receive 277CA claim acknowledgments after you submit 837 claims through Stedi.
These 277CAs indicate whether the claim was accepted for processing or rejected. If the claim was rejected, the 277CA explains why so you can understand what to change before resubmitting.
277CA responses
You may receive multiple separate 277CAs for each claim you submit. Each 277CA typically correlates to one claim. However, some payers may send a single 277CA that references multiple claims.
- You'll receive the first 277CA from Stedi within about 30 minutes of submitting the claim. This 277CA may contain rejection message(s) and warnings, if applicable.
- You may receive additional 277CAs from intermediary clearinghouses.
- You'll receive one or more 277CAs from the payer. Typically, there is one 277CA that indicates receipt of the claim and a second 277CA that contains summary counts of transactions received, information about accepted transactions, and details for rejected transactions.
Review 277CAs
You can find 277CAs related to a specific claim on the Related transactions tab of that claim's details page.

You can also go to the Transactions page and click Filters. To find a specific 277CAs, we recommend the following filters:
| Filter | Description |
|---|---|
| Search term |
|
| Date processed | This is the date Stedi received the 277CA, not the date of service. Make sure you select the correct Time zone at the bottom of the filter. |
| Transaction type | Select 277 Health Care Information Status Notification to show only 277CA transactions. |
Determine claim status
277CAs from the payer indicate whether the claim was accepted for processing or rejected.
This claim status information is available on the 277CA's Overview tab. If the 277CA references multiple claims, you can toggle between them to review each claim's status information.
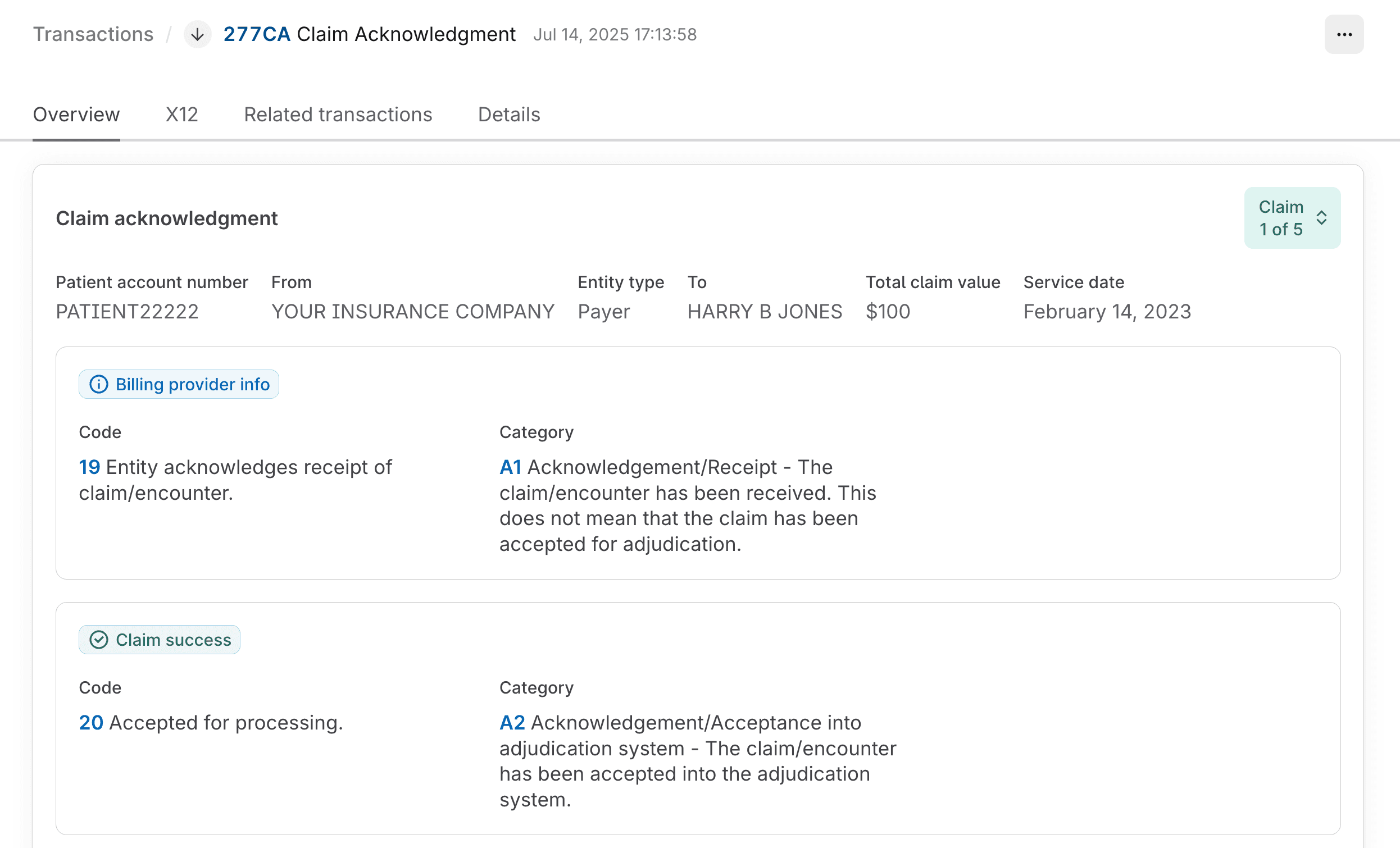
Specifically, you should review the following details:
| Information | Description |
|---|---|
| Sender | The 277CA is from the payer when the From field contains the payer's name or ID and the Entity type is Payer. |
| Patient Account Number | This is the value you sent in the original claim's Loop 2300 CLM01 (Patient Control Number). It can help you match the 277CA to the original claim. |
| Status codes | The overview lists claim status codes that indicate whether the claim has been accepted or rejected. If the claim was rejected, the overview lists one or more rejection messages marked with Claim issue indicating the reason(s) for rejection. |
When the linked claim has been rejected due to one or more Claim issues, you can click Edit and resubmit claim to go directly to the resubmission form for that claim. Visit Revise and resubmit claims for instructions.
Download X12 EDI
You can review and download the raw X12 EDI for any 277CA claim acknowledgment from the X12 tab.
The EDI is displayed on the right and the specification is displayed on the left. As you hover over different parts of the EDI, Stedi highlights the corresponding part of the specification to help you understand what each part of the EDI means.
Click the download button (down arrow icon) at the top left of the EDI viewer to download the transaction as an .edi file.
277CA vs. claim status check
The 277CA contains different information than a real-time claim status check. Specifically:
- 277CAs: Tell you whether the payer has received a claim and accepted it for processing. If the claim was rejected, 277CAs tell you why so you can resubmit. 277CAs don't indicate whether the claim has been adjudicated or paid.
- Real-time claim status checks: Tell you the status of a claim that's already been accepted into the payer's system. They provide information about whether the claim has been adjudicated, paid, denied, or is pending further review.
If you're waiting for an ERA, you should first check the related 277CA to confirm that the claim was accepted for processing. If the claim was rejected, you won't receive an ERA because the payer didn't adjudicate the claim.
Then, you can run a real-time claim status check to get updates about the claim's adjudication and payment status.