Review and resubmit claims
You can review, revise, and resubmit claims in the Stedi portal. This includes professional claims you submitted through the portal as well as professional, dental, and institutional claims third-party vendors submitted through Stedi on your behalf.
You may need to resubmit claims for several reasons, including changes to the patient's coverage, errors in the original claim's information, or appealing a denied claim. You may also need to cancel duplicate claims or claims that were submitted in error.
Find specific claims
The Transactions page shows all submitted 837 claims, 277CA claim acknowledgments, and 835 Electronic Remittance Advice (ERA) responses.
Click Filters to narrow the list to specific claims. We recommend the following filters:
| Filter | Description |
|---|---|
| Search term | We recommend entering the claim's Patient Control Number (Loop 2300 CLM01) if it's unique for each claim. This will help you find the specific claim you're looking for. If you don't have the Patient Control Number, you can search for another identifier, such as the patient's member ID or last name, to help narrow down the results. The search term must match what's in the claim exactly, including all spaces, capitalization, and punctuation. |
| Date processed | This is the date Stedi received the claim, not the date of service. Make sure you select the correct Time zone at the bottom of the filter. |
| Transaction | Select 837 Health Care Claim to filter for only submitted claims. Stedi will show all claim types - professional, dental, and institutional (if present) in the filtered list. |
Once you find the transaction you want to review or resubmit, click it to open its details page.
Revise and resubmit claims
You can manually revise and resubmit professional, dental, and institutional claims in the Stedi portal. The resubmission process is the same for both corrections and cancellations - the Claim Frequency Code indicates which action you want to take.
- For professional claims, you can edit and resubmit through either the interactive CMS-1500 form or the X12 EDI editor.
- For dental and institutional claims, you can only edit and resubmit through the X12 EDI editor.
CMS-1500 form (professional)
Stedi's CMS-1500 claim form UI is mostly limited to the CMS-1500 form fields. It may not be able to successfully resubmit complex claims originally submitted through our APIs or SFTP.
To resubmit a professional claim through Stedi's interactive CMS-1500 form:
- Go to the Transactions page and click the claim you want to resubmit to open its details page.
- Click Edit and resubmit and select 1500 resubmission. Stedi opens the interactive CMS-1500 form prepopulated with the claim's information.
- Make any necessary changes to the claim.
- Make sure to update the Claim Frequency Code, the Payer Claim Control Number, and the Patient Control Number according to best practices.
- You can click Related transactions to review related 277CAs containing the errors you need to address before resubmitting. Click a transaction to review its details.
- Click Submit claim to resubmit the updated claim to the payer.
Stedi validates the updated claim and submits it to the payer. It will appear on the Transactions page as a new 837 claim. You will also receive new 277CA claim acknowledgments indicating whether the resubmitted claim was accepted or rejected.
X12 EDI editor
To resubmit a professional, dental, or institutional claim through Stedi's X12 EDI editor:
-
Go to the Transactions page and click the claim you want to resubmit to open its details page.
-
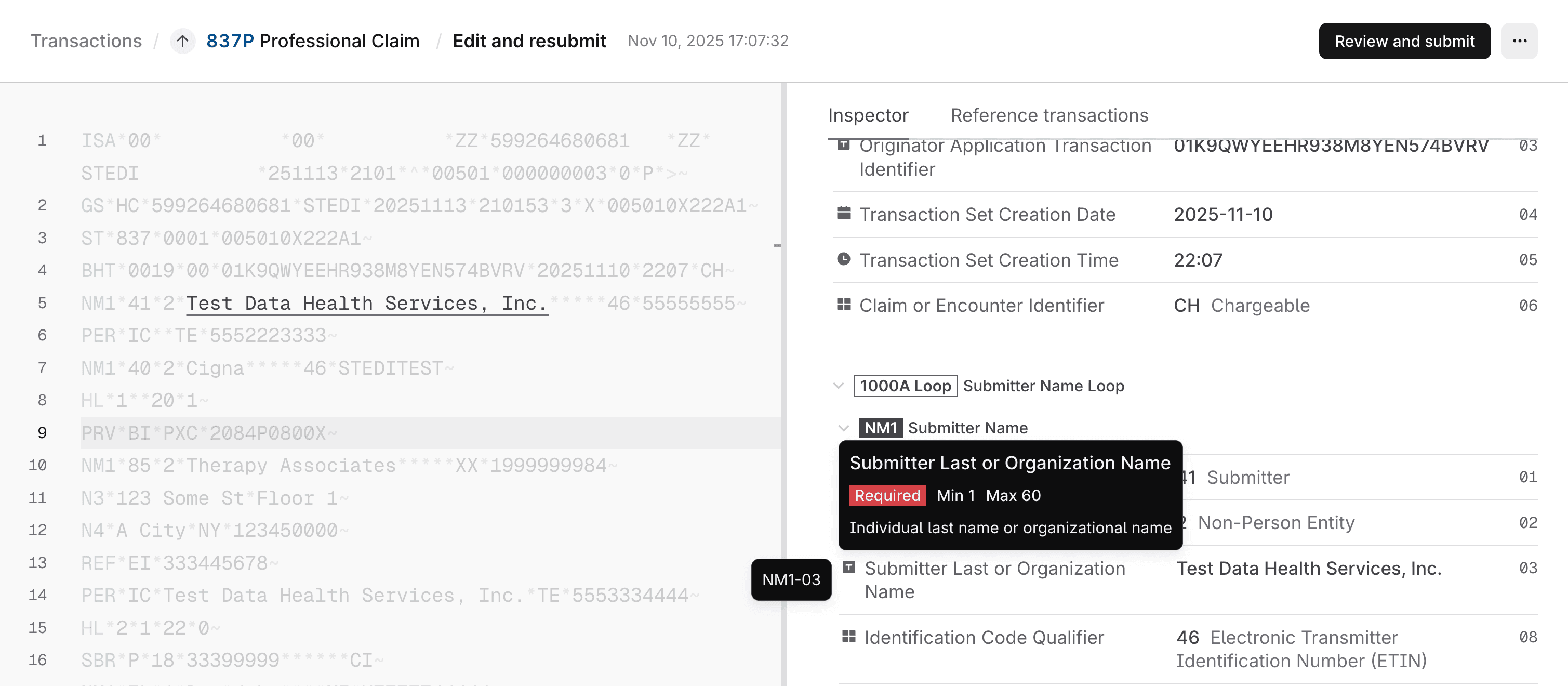
Click Edit and resubmit and select X12 EDI resubmission. Stedi opens the claim in an interactive editor with the X12 EDI on the left and the EDI specification on the right.
As you hover over different parts of the EDI, Stedi highlights the corresponding part of the specification in the Inspector tab to help you understand what each part of the EDI means and how to edit it correctly.
-
Make changes to the claim EDI.
- You can type directly in the EDI editor or copy and paste updated EDI from another source.
- Make sure to update the Claim Frequency Code, the Payer Claim Control Number, and the Patient Control Number according to best practices.
- You can switch to the Reference transactions tab to review related 277CAs containing the errors you need to address before resubmitting. Click a transaction to review its details.
-
Click Review and submit. Stedi shows a comparison of the original claim and the new claim containing your changes.
-
Click Resubmit claim to send the updated claim to the payer.
Stedi validates the updated claim and submits it to the payer. It will appear on the Transactions page as a new 837 claim. You will also receive new 277CA claim acknowledgments indicating whether the resubmitted claim was accepted or rejected.
Resubmission best practices
To revise or cancel a claim, you'll need to resubmit the claim with:
- The proper Claim Frequency Code
- The original claim's Payer Claim Control Number (if available)
- A new, unique Patient Control Number (PCN)
- Any other necessary corrections
Claim Frequency Code
You must choose the correct Claim Frequency Code when correcting or canceling claims. The Claim Frequency Code is represented as the:
Loop 2300 CLM05-03(Claim Frequency Code) component in X12 EDI.- Resubmission code (Box 22) in Stedi's CMS-1500 claim form UI.
The right Claim Frequency Code depends on where the claim is in the processing lifecycle. Specifically, you should only use Claim Frequency Code 7 (Replacement of Prior Claim) or 8 (Void/Cancel of Prior Claim) if the claim has already entered the payer's processing system. You'll know the claim has entered the payer's system if the 277CA contains a Payer Claim Control Number (PCCN).
The following diagram shows how claims can be rejected by Stedi or the payer at different stages in the processing lifecycle and when to use each Claim Frequency Code.
Choose the right code
The following guidance can help you determine which Claim Frequency Code is right for your use case. These rules apply to professional, institutional, and dental claims for most payers.
Some payers have different rules. For example, Medicare only accepts code 1 for resubmissions. Always adhere to the payer's specific guidance when resubmitting or canceling claims.
| Scenario | How you'll know | Claim Frequency Code |
|---|---|---|
| Stedi rejected the claim due to validation errors | You received a 277CA claim acknowledgment from Stedi with rejection status codes. | 1 - Admit thru Discharge Claim |
| Payer rejected the claim without processing it | You received a 277CA from the payer with rejection status codes. The payer may include a message, such as "returned as unprocessable" or "not entered into processing system." The 277CA doesn't contain a Payer Claim Control Number (PCCN), which means it hasn't entered the payer's processing system. | 1 - Admit thru Discharge Claim |
| Payer rejected the claim after it entered their processing system | You received a 277CA from the payer with rejection status codes. The 277CA contains a Payer Claim Control Number (PCCN), indicating it has entered the payer's system. | 7 - Replacement of Prior Claim (except Medicare) |
| You need to correct and resubmit an adjudicated claim (approved, pended, or denied) | You received an 835 Electronic Remittance Advice (ERA) from the payer with adjudication details for the claim. | 7 - Replacement of Prior Claim (except Medicare) |
| You need to completely cancel a claim in the payer's processing system | You received an 835 Electronic Remittance Advice (ERA) or you have received a 277CA (acceptance or rejection) containing a Payer Claim Control Number (PCCN). | 8 - Void/Cancel of Prior Claim |
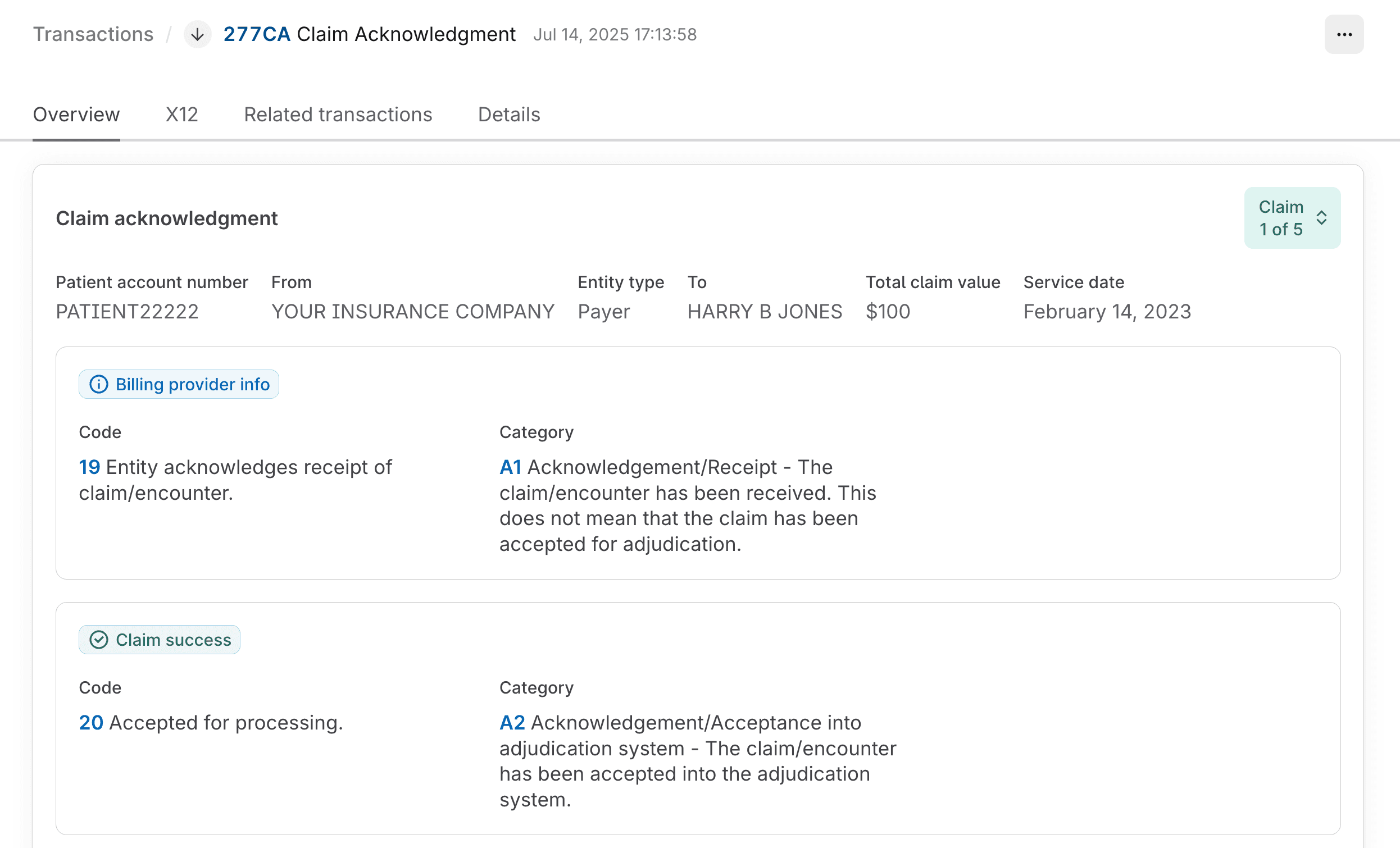
Determine 277CA sender
To select the right Claim Frequency Code, you'll need to know whether the 277CA rejection came from Stedi or the payer. You can determine who sent a 277CA:
- Go to the Transactions page.
- Click the 277CA you want to review.
At the top of the details page, the From and Entity type fields indicate whether the acknowledgment is from Stedi or the payer.
Payer Claim Control Number (PCCN)
When you're resubmitting with Claim Frequency Code 7 or canceling with Claim Frequency Code 8, you must include the original claim's Payer Claim Control Number (PCCN). Without it, the payer won't know which claim to replace or cancel.
You can include the PCCN in Loop 2300 REF02, where REF01 = F8 (Original Reference Number).
An exception to this general rule is Medicare, which explicitly instructs providers to omit the PCCN when resubmitting claims. Visit Medicare resubmission for details.
Where to find the PCCN
You can retrieve the Payer Claim Control Number (PCCN) for the original claim from any of the following transactions from the payer.
| Transaction | How to get it |
|---|---|
| 277CA claim acknowledgment | Go to the X12 tab and check the value in Loop 2200D REF02 (Payer Claim Control Number), where REF01 = 1K (Payor's Claim Number). |
| 277 real-time claim status | Run a claim status check for the claim you want to resubmit. The PCCN is available on the results page as Payer claim control number. |
| 835 Electronic Remittance Advice (ERA) | Go to the Overview tab. The PCCN is labeled as the Payer claim number in the claim identifiers column. |
The PCCN is different from the Patient Control Number (Loop 2300 CLM01) you sent in the original claim.
Patient Control Number
When resubmitting claims with any Claim Frequency Code (1, 7, or 8), we strongly recommend setting a new, unique Patient Control Number (PCN).
The value you supply will be present in both the 277CA and the 835 ERA responses, allowing you to correlate the resubmitted claim with its responses later. You can set the PCN in the following locations:
Loop 2300 CLM01(Patient Control Number) in X12 EDI.- Patient account number (Box 26) in Stedi's CMS-1500 claim form UI.
When assigning a PCN, follow these best practices:
- Use a unique PCN for each claim. The identifier should be more complex than a simple sequential number and should be hard to guess.
- Use random strings. Formats with patient initials or the date of service in them can create duplicates. We recommend using nanoid or a similar library to create a strong, unique 17-character PCN for each claim.
- Keep it 17 characters or less. Some payers cut off values longer than 17 characters in ERAs and claim acknowledgments, which makes it hard to match them with the original claim.
- Use alphanumeric characters only. Avoid special characters, as many payers don't handle them properly.
Medicare resubmission
Medicare (through MACs) has different requirements for resubmissions and cancellations:
- Only resubmit with Claim Frequency Code
1. Medicare does not accept Claim Frequency Code7for resubmissions. - Don't include the original claim's Payer Claim Control Number (PCCN) when resubmitting.
