Transaction enrollment overview
Transaction enrollment is the process of registering a provider to exchange:
- a specific healthcare transaction (like 835 Electronic Remittance Advice ERAs)
- with a specific payer (like Cigna or UnitedHealthcare)
- through a specific clearinghouse (Stedi).
When a payer requires transaction enrollment, you must complete the process before you can begin exchanging that transaction type through Stedi. It typically takes 24-48 hours.
Do I need to enroll?
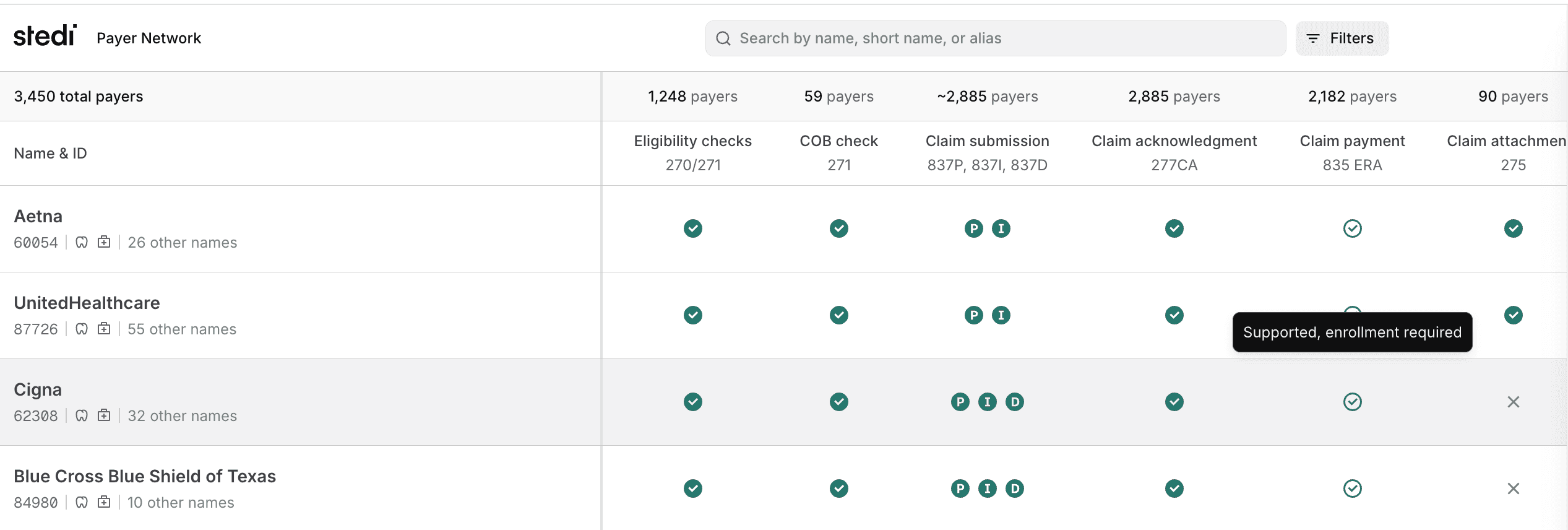
All payers require transaction enrollment for 835 Electronic Remittance Advice (ERAs). For other transactions, like claims and eligibility checks, it depends on the payer.
Check the Payer Network to determine whether your payers require enrollment for the transaction types you want to send and receive. For transactions marked as Supported, enrollment required, you must complete the transaction enrollment process before you can begin exchanging that transaction type through Stedi.
Transaction enrollment is specific to each clearinghouse. If you're already enrolled with a payer through another clearinghouse, you still need to complete enrollment with Stedi.
Don't enroll for 835 ERAs until you're ready to switch to Stedi. Once you enroll, all ERAs from that payer will come through Stedi exclusively. You'll no longer receive ERAs from that payer through your previous clearinghouse.
Transaction enrollment process
Stedi handles most of the transaction enrollment process for you. Here's how it works:
You can submit transaction enrollment requests either individually or in bulk through CSV import. With both methods, you'll:
- Create a provider record with the billing provider's tax ID, NPI, and contact information.
- Submit enrollment requests containing the provider record, the payer, and the transaction type.
When we begin the enrollment process with the payer, we'll set the enrollment status to PROVISIONING. You'll get notification emails each time the status changes or there is new information for you to review.
For some payers, such as those with one-click enrollment, Stedi can complete the entire enrollment process for you. We sign enrollment PDF forms on your behalf, when possible, to speed up the process and eliminate extra work for your team.
Some enrollments may require you to complete additional steps. If there are additional steps, we'll set the enrollment status to PROVIDER ACTION REQUIRED and add a task to the enrollment request with clear instructions. The enrollment process continues once you complete the required tasks.
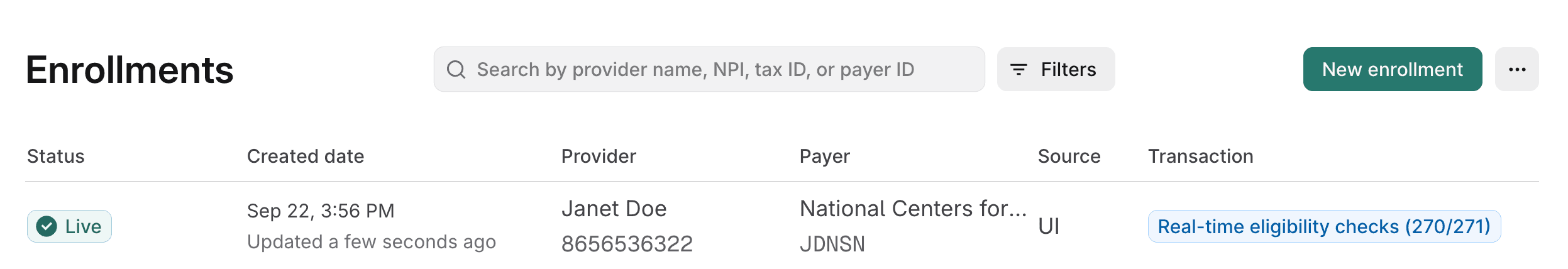
Once a transaction enrollment request is in LIVE status, you can start exchanging that transaction type through Stedi.
ERAs can only be sent to one clearinghouse, so you'll start receiving them through Stedi exclusively. Your enrollment with any other clearinghouses will be canceled.
For other transaction types, like claims and eligibility checks, you may be able to continue sending them through other clearinghouses - it depends on the payer.
Check out our Enrollment FAQ for answers to common questions.