Review patient benefits
You can review the results of successful eligibility checks to determine whether a patient's health plan covers the requested services. You can also view details about specific benefits, such as co-pay amounts, deductible information, and whether prior authorization is required.
Eligibility check results
To review an eligibility check's results:
- Go to the Eligibility searches view.
- Click the eligibility search with the patient information you want to view.
Stedi opens the eligibility search's Overview tab.
Overview tab
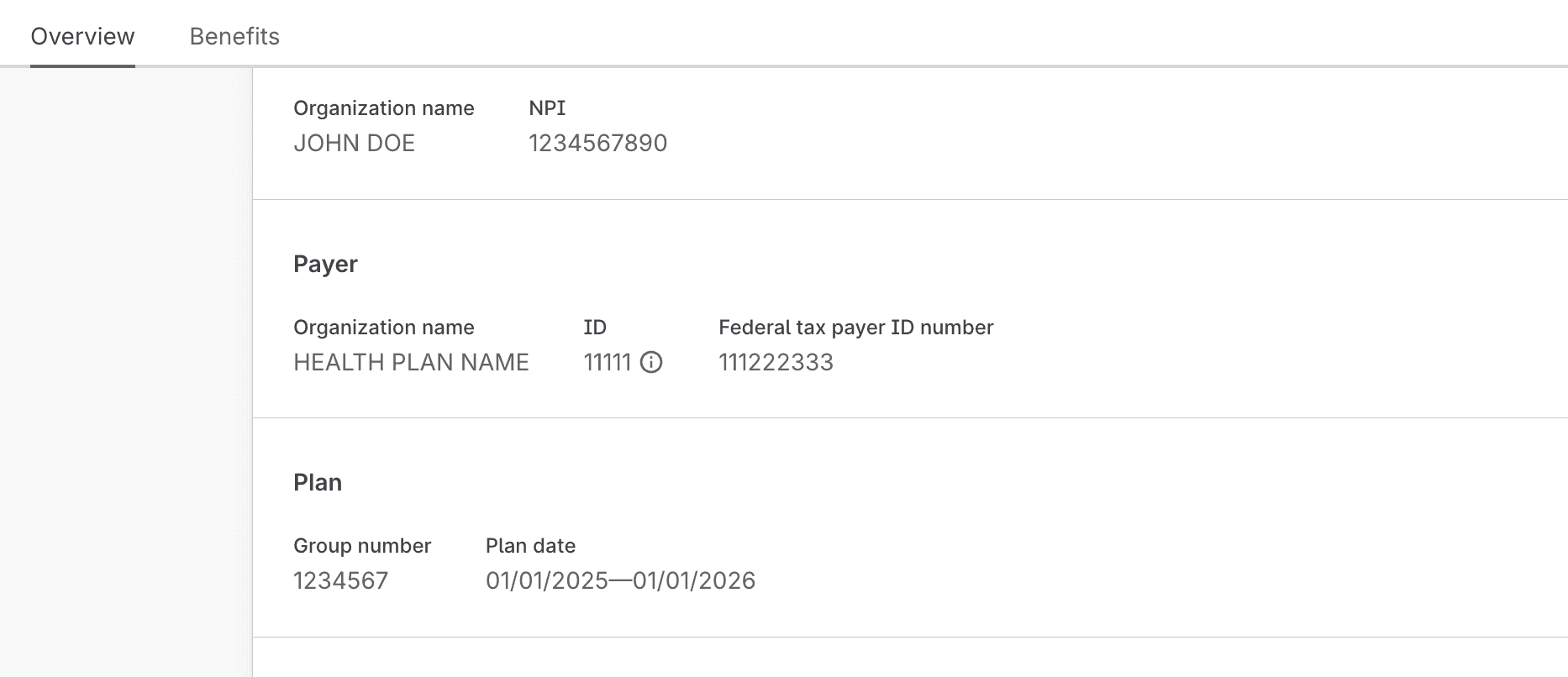
The Overview tab shows details about the latest eligibility check in the eligibility search.

If the eligibility check was successful, the Overview tab contains:
- Patient information, such as their name, date of birth, and member ID.
- The service type code(s) you requested.
- The requesting provider's information, including their name and NPI.
- The payer's information, including their name and Payer ID.
- The patient's health plan information, including the plan names, group number, and plan begin and end dates.
- Any benefits related entities, which are commonly used to designate the patient's primary care provider (PCP), another organization that handles a specific carveout benefit type (such as telehealth mental health services), or another health plan for the patient (coordination of benefits scenarios).
Benefits tab
The Benefits tab displays the patient's benefits in filterable table. Information in the table is grouped into sections:
- The first grouping mechanism is the patient's health plan. Many eligibility responses only contain benefits for a single health plan, but some responses include benefits for multiple plans. For example, if the patient has both a primary health plan and a dental plan, the benefits view will contain separate sections listing all of the benefits for each plan.
- Within each health plan section, benefits are further grouped by service type code (STC) and procedure code so that you can easily find and review all of the benefits for a specific set of services.

There may be multiple benefits for the same STC and benefit type. For example, a patient may have different co-insurance amounts for in-network and out-of-network providers or for specific services within a broader STC. The Messages field contains notes from the payer, which typically list limitations or conditions that apply to the benefit.
In the following example, the patient has a $200 co-pay for Emergency Services (STC 86), but the messages indicate that this co-pay is waived if the patient is admitted to the hospital.

Benefits filters
Payers typically send more benefits information than you requested. You can filter the benefits table by the following criteria to review only the benefits you care about. The options for each filter type depend on the benefits data in the payer's response. For example, if the payer didn't return any family-level benefits, the Coverage level filter won't have a Family option.
| Filter | Description |
|---|---|
| Type | This is the benefit type code, such as Co-insurance or Deductible. |
| Coverage level | The coverage level. This is typically either Individual or Family, but the values can vary depending on the patient's plan. |
| Network | Whether the benefit applies to in-network providers, out-of-network providers, or both.
|
| Service or procedure | The service type code (STC) or procedure code associated with the benefit. For example, UC for Urgent Care or MH for Mental Health. |
| Place of service | The names of place of service codes associated with the benefit. For example, Emergency Room - Hospital for service type code 23. |
| Message | Messages from the payer associated with the benefit. For example, Co-pay waived if admitted. |
| Plan name | The name of the patient's health plan. |
For example, to determine the patient's co-pay for urgent care visits with in-network providers, you might set the Type filter to Co-payment, the Network filter to In-Network, and the Service or procedure filter to UC or another relevant code.
Does the patient have coverage?
The patient has coverage when the date of service is within the plan's eligibility period, and the patient has active coverage for the relevant services. Here's how to check whether these conditions are met:
- Go to the Overview tab of an eligibility search.
- Review any available Plan begin and/or Plan end dates.
If the date of service is within that range, the patient may have coverage.
- Go to the Benefits tab.
- Filter by Service / procedure and choose the STC(s) or procedure code(s) you care about.
The Status field in the Benefit column may show whether the patient has active coverage for the relevant STC(s) or procedure code(s). Typically, only broad STCs (30 and 35 for general medical and dental coverage) will have a status.
- The patient has coverage when the status is Active coverage for the relevant STC or procedure code. You can also assume the patient has coverage when there is no status, but benefits are listed (such as co-pay or deductible amounts).
- The patient doesn't have coverage when the status is Inactive for an STC or procedure code. You can also assume the patient doesn't have coverage if there are no benefits listed or the payer returned a message indicating that the service isn't covered.

Eligibility searches have an Active status when the latest eligibility search in the record returned at least one active benefit type. However, you must review the benefits table to confirm that the patient has active coverage for the STCs you care about.
What is the patient's financial responsibility?
Once you've confirmed that the patient has coverage, you may want to understand their financial responsibility for services. For example, you may want to know their co-pay amount for an in-office visit or whether they've met their deductible.
You can use the Type filter on the Benefits tab to narrow the results to specific benefits types (such as co-pay amounts) for each STC or procedure code.
The following example shows that the patient has a 20% co-insurance for diagnostic lab services (STC 5) with out-of-network providers when those services are performed in a hospital emergency room (place of service code 23).

Is the provider in- or out-of-network?
Unfortunately, you can't reliably answer this question from a standard eligibility response.
Payers typically don't explicitly indicate whether the requesting provider is in- or out-of-network for the patient (though there are some exceptions). The Network indicator field in the table only indicates whether the benefit applies to in-network or out-of-network providers in general. It doesn't tell you whether the requesting provider is in- or out-of-network for the patient.
Some payers do provide additional information about whether the requesting provider is in- or out-of-network. They may do this through either freeform messages or selective inclusion of benefits in the response.
For example, some payers only return out-of-network benefits if the requesting provider is out-of-network. Likewise, if the provider is in-network, they only provide in-network benefits. Stedi doesn't have a complete list of payers that selectively include or exclude benefits based on the provider's network status.
The most reliable way to determine network status is to check directly with the payer or the provider. Note that payers may have different networks for different health plans, such as employer-sponsored plans versus Medicare Advantage, and these networks may have different contact paths.
Is prior authorization required?
Prior authorization (also called pre-authorization or pre-certification) is a requirement that the patient or their provider must get approval before a payer will cover specific services, procedures, medications, or devices. Without it, the payer may deny claims.
If the payer provides prior authorization information in the eligibility response, it will be listed in the Benefit column for that service or procedure. The payer may also send messages in the Messages field about prior authorization rules.

If the payer doesn't provide prior authorization information for a service or procedure, you can assume that prior authorization isn't required.