Run eligibility checks
You can run both real-time and batch 270/271 eligibility checks in your account to verify a patient's insurance coverage and benefits.
You can also run a special kind of real-time eligibility check called a Medicare Beneficiary Identifier (MBI) lookup. MBI lookups allow you to retrieve benefits information from the Centers for Medicare and Medicaid Services (CMS) when you don't know the patient's MBI.
Real-time eligibility checks
Real-time eligibility checks provide a response in seconds. They're ideal for in-person patient visits, telehealth appointments, and other scenarios where you need immediate information about a patient's coverage.
To run a new eligibility check:
- Go to the Eligibility searches view.
- Click + New eligibility check.
- Enter the required information.
- We recommend starting with the default form fields, but you can click Select fields to include additional information, such as dependent information or service dates. Review basic eligibility request fields for detailed instructions and tips for completing the form.
- Choosing the right service type code (STC) or procedure code is very important for getting the best results from the payer.
- We recommend submitting one STC per request, unless you've tested and are certain that the payer supports multiple.
- To request general medical benefits, we recommend using STC
30(Health Benefit Plan Coverage). - To request general dental benefits, we recommend using STC
35(Dental Care). - When requesting benefits for specific services, you should test the STCs that seem most appropriate to determine which ones yield the most benefits information. Our docs for choosing the right STCs and procedure codes explain how.
- Click Submit.
Stedi runs the eligibility check and stores it in a new eligibility search. Stedi automatically opens the Eligibility search overview page for the check.
Click View to see the details of the eligibility check, including a benefits summary if the check was successful. If the check failed, you can review the error code and retry the check with updated information. Visit Fix failed eligibility checks for instructions.
MBI lookup
A Medicare Beneficiary Identifier (MBI) is a unique, randomly-generated identifier assigned to individuals enrolled in Medicare. You must include the patient's MBI in every eligibility check you submit to the Centers for Medicare and Medicaid Services (CMS).
When patients don't know their MBI, you can perform an MBI lookup instead of a standard eligibility check. You can run MBI lookups through the eligibility check form or through bulk CSV upload.
Types of MBI lookups
There are two types of MBI lookups you can perform with Stedi. For each, you'll use a special payer that tells Stedi to perform an MBI lookup for the patient in addition to a standard eligibility check.
| Type | What's required | Payer |
|---|---|---|
| With SSN | first name, last name, date of birth, Social Security Number (SSN) | CMS MBI Lookup |
| No SSN | first name, last name, date of birth, U.S. state | CMS MBI Lookup Without SSN |
We recommend running MBI lookups with the patient's SSN whenever possible. When the SSN is present, the MBI lookup has a higher likelihood of successfully returning their MBI. MBI lookups with no SSN are a fallback option when the patient's SSN isn't available.
You don't need to include more patient demographic information than what's required, such as additional address data. It doesn't improve MBI lookup success rates.
Run an MBI lookup
To run an MBI lookup:
-
Go to the Eligibility searches view and click + New eligibility check.
-
Construct an eligibility check request with the required patient demographic data. You don't need to include more than the required fields, such as extra address data. Extra demographic data won't improve lookup success rates.
-
With SSN: Include the patient's first name, last name, date of birth, and SSN.
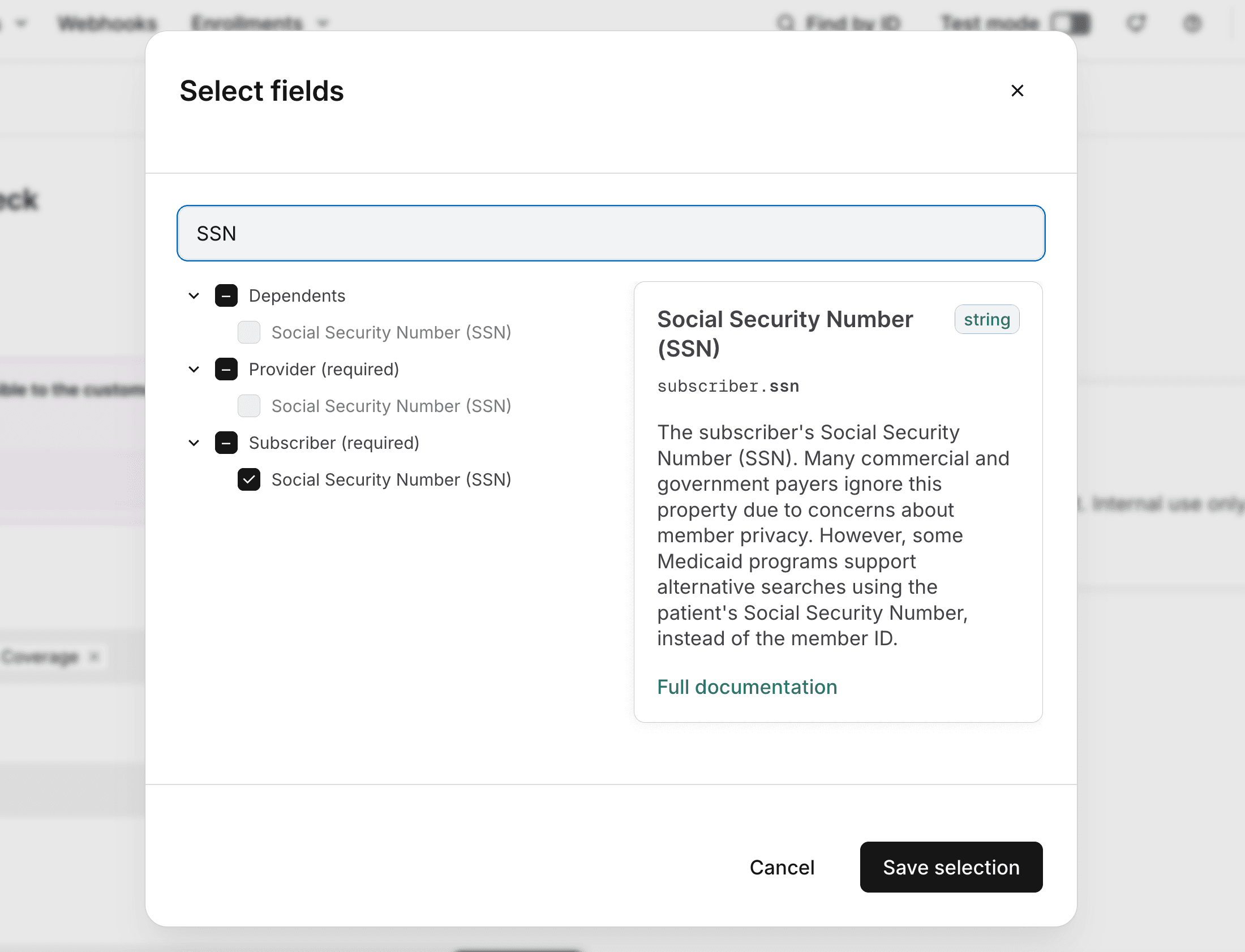
You'll need to click Select fields and check the box next to Social Security Number (SSN) under the Subscriber section. This adds the SSN field to the form.
-
No SSN: Include the patient's first name, last name, date of birth, and U.S. state.
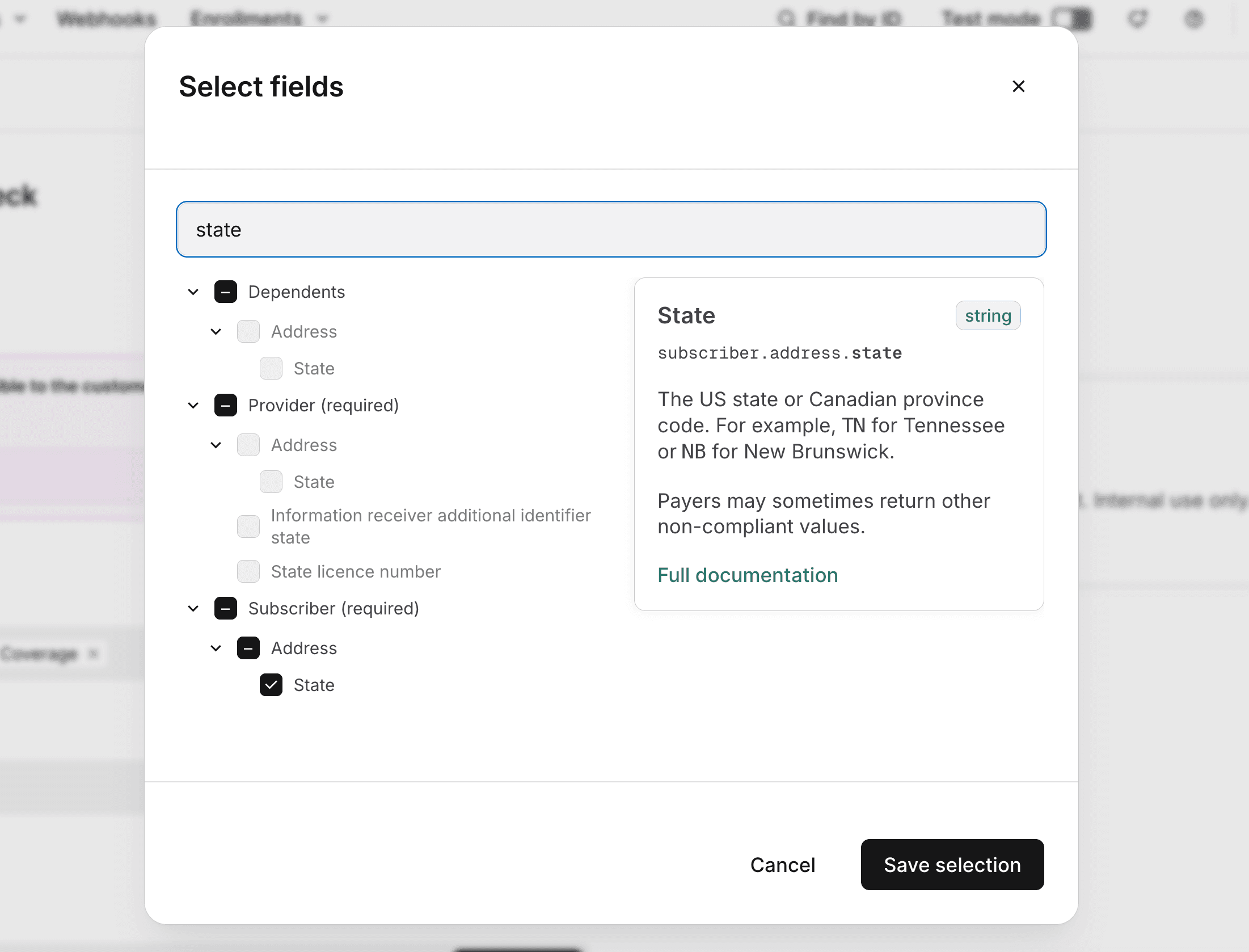
You'll need to click Select fields and check the box next to State under the Subscriber > Address section. This adds the State field to the form. You can leave the rest of the address fields blank.
-
-
Set the Trading partner service ID to either:
- CMS MBI Lookup for MBI lookups with SSN.
- CMS MBI Lookup Without SSN for MBI lookups without SSN.
-
Enter the rest of the required information. Review basic eligibility request fields for detailed instructions about how to complete the Provider and Encounter sections.
-
Click Submit.
Stedi uses the patient's demographic data and SSN to perform an MBI lookup. If there is a match, Stedi submits an eligibility check to CMS. Stedi returns a complete eligibility response from CMS for the patient and returns the patient's MBI as the subscriber's member ID.
Stedi automatically opens the Eligibility search overview page for the MBI lookup when it's complete.
Medicare Advantage plans have their own unique member ID, which isn't returned in the MBI lookup response. You also shouldn't submit eligibility checks for Medicare Advantage plans to CMS (HETS) - you should submit them to the actual Medicare Advantage plan payer instead.
Outdated MBI error
Stedi's MBI lookup may rarely retrieve an outdated MBI for a patient. CMS may rotate an MBI for a member for various reasons at any time, such as to help protect against identity theft.
In these cases, the response will contain an AAA error with code 72 (Invalid/Missing Subscriber/Insured ID) and return a subscriber member ID, which is the outdated MBI.

Batch eligibility checks
We recommend using batch checks for bulk workflows that aren't time sensitive, such as monthly or weekly eligibility refreshes. You can submit batch eligibility checks and MBI lookups through bulk CSV upload.
Create new CSV batch
To create a new CSV batch:
- Go to the Batch eligibility checks page.
- Click + New batch from CSV.
- Enter a unique name for the batch. Stedi displays this name in the list of batch uploads. This name is for your reference only - we don't send it to payers.
- (Optional) Click Advanced options to configure a custom Retry duration between 8 and 24 hours. This is the maximum number of hours that Stedi will retry checks in the batch that fail due to payer connectivity issues. The default is 8 hours.
- Click Create to go to the CSV upload page for your new batch.
Upload CSV file
On the CSV upload page for your batch:
-
Click Download a template to download the CSV template with the supported fields. You can also download it from this link: template CSV file.
-
Populate the template with eligibility checks. Each row in the template represents one eligibility check. You can submit up to 10,000 checks per CSV file. The upload page contains detailed documentation for each possible field and recommendations for which fields to include for the best chance of success.
You can also submit MBI lookups through CSV upload. Set the
tradingPartnerServiceIdfor each check to either MBILU (for MBI lookups with SSN) or MBILUNOSSN (for MBI lookups without SSN). Then, include the required patient demographic information for each lookup. -
Click + Upload file to upload your complete CSV file.
-
Click Verify file so Stedi can validate the data in each eligibility check. You can fix any errors and re-upload the CSV file as many times as needed. When the file is error-free, you'll be able to execute the batch.
-
Click Execute batch to send the eligibility checks to Stedi for processing.
Stedi begins processing the batch. Each eligibility check in the batch is stored in its own eligibility search. You can review the details of each check from the Eligibility searches view.
Review batch progress
You can review the progress of submitted batches on the Batch eligibility checks page. The page displays each CSV batch you've submitted, along with it's name, date created, status, and total items (number of eligibility checks in the batch).
- The batch status changes to In progress while Stedi is processing the batch.
- The batch status changes to Completed when Stedi has sent all checks in the batch to payers and received responses.
- Most batches complete in 15 to 30 minutes. However, Stedi retries checks that fail due to payer connectivity issues for up to the configured retry period, so it can take up to the end of the retry period for all checks in a batch to return results.
Click a batch to view its details, including the status of each check in the batch. Click any eligibility check to go to its details page.
From the batch details page, you can also download the original CSV input by clicking Download under Original input file.
Basic eligibility request fields
For the best chance of success, start by sending the smallest possible set of fields in your eligibility checks. Adding extra data can lead to unnecessary rejections.
We recommend starting with the following information. Only include more if the payer requires it.
| Information | Instructions |
|---|---|
| Encounter, service or procedure codes | You must include either a service type code (STC) or a procedure code and qualifier. This tells the payer what kinds of benefits information you're requesting. Most medical payers don't support procedure codes. Some dental payers do, but we recommend trying an STC first.
|
| Encounter, service dates | Stedi uses the today's date in the payer's timezone as the date of service by default. If you want to check eligibility for today's date, don't submit a service date.
|
| Subscriber |
|
| Dependents | A patient qualifies as a dependent for eligibility checks when they are listed as a dependent on the subscriber's insurance plan and the payer cannot uniquely identify the patient through information outside the subscriber's policy. If the patient has their own member ID (even if it only differs by a suffix like 0), you must identify them in the Subscriber section instead.
|
CMS HETS Rules of Behavior
All parties involved in eligibility transactions sent to the Centers for Medicare & Medicaid Services (CMS) eligibility system, called HETS, must comply with the HETS Rules of Behavior. Compliance is also required under our terms.
Review the Rules of Behavior before sending eligibility checks to CMS.