Test claims workflow
You can submit test professional, dental, and institutional claims to make sure your claims process is working smoothly from end to end. When you submit test claims to the Stedi Test Payer, Stedi generates and returns an 835 Electronic Remittance Advice (ERA) based on the original claim.
Submit test claims
You can submit test claims with any payer ID and receive test 277CA claim acknowledgments from Stedi. This helps you test your claim submission workflow and practice interpreting and handling 277CA responses.
To send a test claim:
- In the 1500 claim form, select Test for the EDI mode.
- During X12 EDI upload, select Test from the dropdown at the top of the text area.
When you send a test claim, Stedi doesn't send it to the payer. Instead, it processes the claim as if it were sent to the payer and returns a 277CA claim acknowledgment response indicating whether the claim was successfully processed.
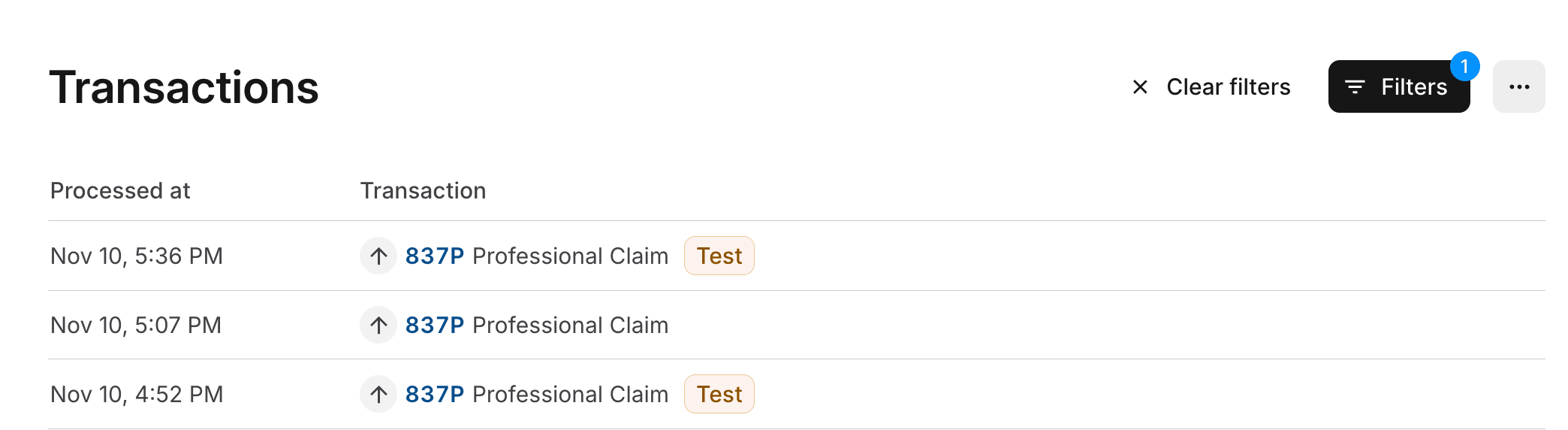
Designating a claim as test data also allows you to filter for test claims on the Transactions page in the Stedi portal. The following example shows the Transactions page filtered to show only 837 claims. There are two test claims (indicated by the Test badge) and one production claim.
Generate test ERAs
When you submit test claims to the Stedi Test Payer, Stedi returns a test 277CA claim acknowledgment and a test 835 Electronic Remittance Advice (ERA) based on the original claim. Only test claims you send to the Stedi Test Payer will generate a test 835 ERA.
You can use this approach to test your claims processing workflow from end to end.
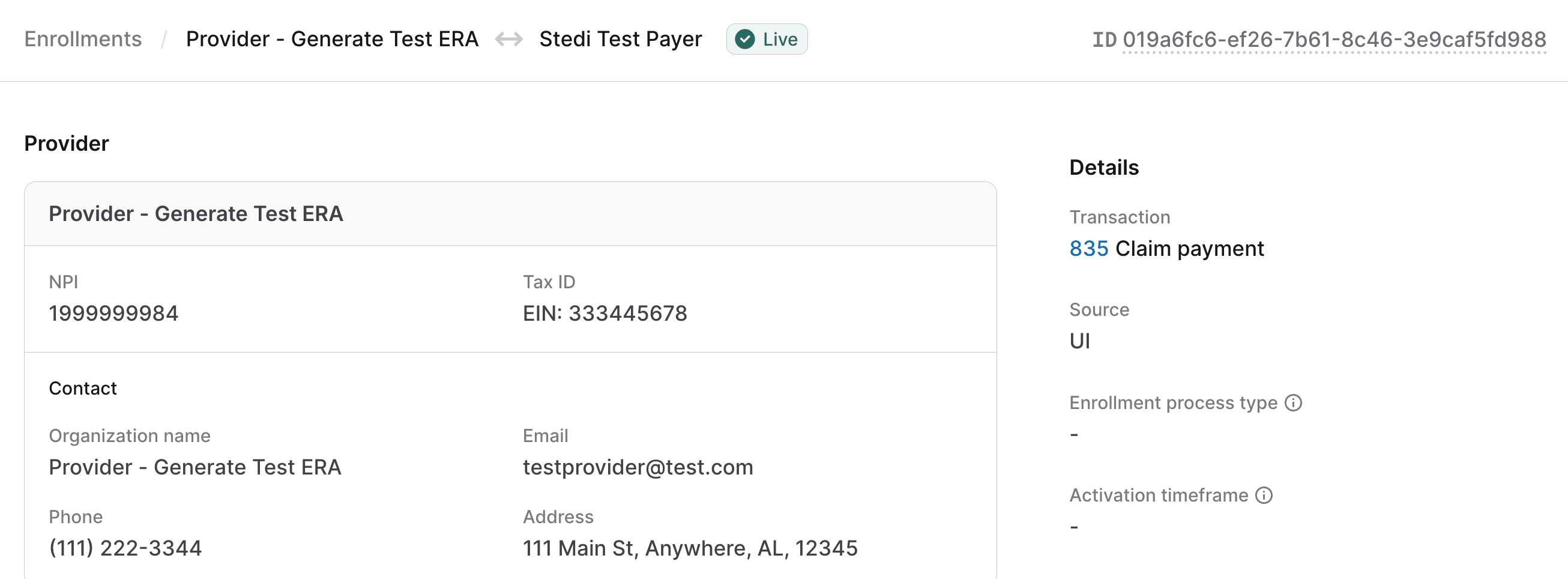
Enroll with the Stedi Test Payer
You must enroll your provider with the Stedi Test Payer for 835 Claim payment. Visit Transaction enrollment for instructions on how to submit an enrollment request.
Once submitted, the enrollment request is automatically set to LIVE status within one minute. You can start submitting test claims to the Stedi Test Payer immediately after enrollment.
Submit a test claim
Submit a test claim to the Stedi Test Payer. Ensure that you:
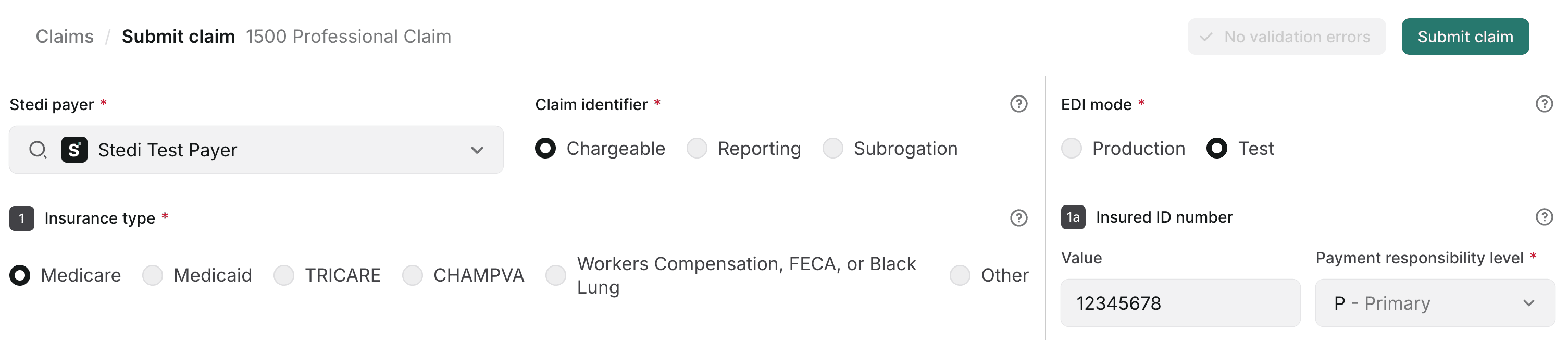
- Designate the claim as test data:
- Select Test for the EDI mode in the 1500 claim form.
- Set
ISA15(Interchange Usage Indicator) toT(Test Data) during X12 EDI upload.
- Set the payer to the Stedi Test Payer.
- Use the billing provider NPI and tax ID you enrolled with the Stedi Test Payer.
The following example shows how to submit a test professional claim to the Stedi Test Payer using the CMS-1500 claim form in the Stedi portal.
Test responses
Stedi returns the following responses within minutes of submitting a test claim to the Stedi Test Payer:
- A test 277CA claim acknowledgment response indicating whether the claim was successfully processed. Note that if Stedi rejects the claim in the 277CA, you won't receive a test 835 ERA.
- A test 835 Electronic Remittance Advice (ERA) containing information from the original claim, including the same:
- Provider information
- Patient information
- Service line details
- Charges
Test 835 ERAs always indicate that all service lines are paid, with the same charge amounts you submitted in the test claim. Note that when you submit real claims, payers may send ERAs with different outcomes, including partially paid, denied, split, or bundled claims.
Review test responses
To review test 277CA and 835 ERA responses, you can either:
- Go to the Transactions page and click the relevant transaction to view its details.
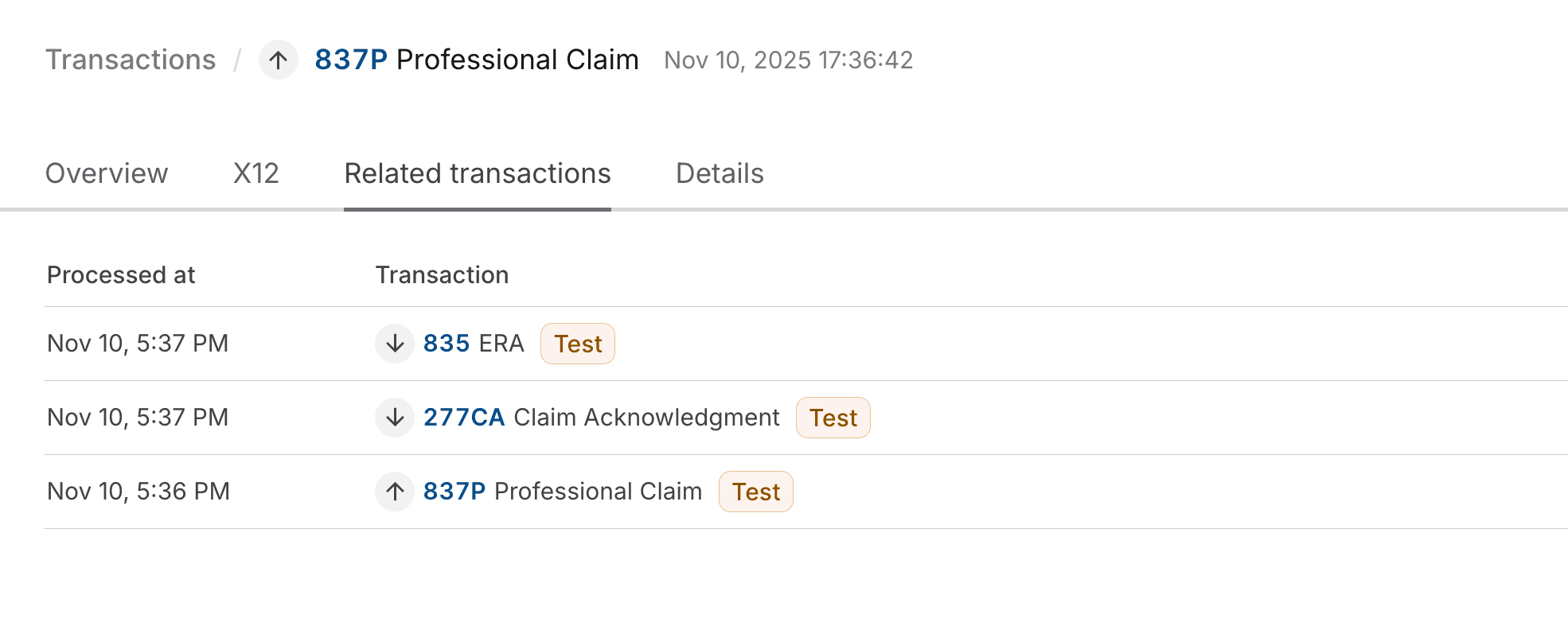
- Go to the Related transactions tab of the test 837 claim submission. Click the test 277CA and test 835 ERA to view their details.
The following example shows the Related transactions tab of a test 837 claim submission, with links to the associated test 277CA and test 835 ERA.
Both the test 277CA and the test 835 ERA will include the Patient Control Number you specified in the claim submission, which is what Stedi uses to match these responses to the original claim.
| Response type | How to find Patient Control Number |
|---|---|
| 277CA | On the Overview tab, the Patient Control Number is displayed as the Patient account number. |
| 835 ERA | On the Overview tab, the Patient Control Number is listed as the first number in the Claim identifiers field. |